Jump to a section below
Key points
- People with intellectual disability speak of the importance of professionals actively working with them and their family, friends and support persons. [1] However, people with intellectual disability and their support networks tell us that professionals often do not collaborate.
- People with intellectual disability and co-occurring mental ill health can have complex and diverse needs.
- These intersecting health, social and disability needs require a co-ordinated cross-sector approach, with active collaboration between service providers within and between sectors.
- When this does not occur, the responsibility often falls to the person, carers and family members to co-ordinate complex care.
- Attitudes and personal views may prevent professionals from including people with intellectual disability in their own care, communicating goals, and working together with other key stakeholders due to different approaches and philosophies.
- The traditional siloing of health, social and disability services after de-institutionalisation has led to a lack of cross-sector collaboration and holistic care. [2] Thus active steps need to be taken by disability and health professionals to provide collaborative care to people with intellectual disability and mental ill health.
Why it is important to work collaboratively
People with intellectual disability, their family and carers, and professionals all bring different knowledge and skills that can be best utilised when everyone works together. Working collaboratively also has the following benefits.
- Reduces barriers faced by people with intellectual disability when accessing services.
- Prevents the person with intellectual disability and their support network needing to repeat their story.
- Allows long-term knowledge (such as a person’s baseline) to be communicated to newer services.
- Ensures consistent understanding of the person’s needs and goals and allows for more efficient care with clearly defined roles.
- Helps to avoid overlap, and ensure complementarity of supports.
- Facilitates clear, non-conflicting advice and treatment or management approaches.
- Provides different perspectives and approaches, which can assist with problem-solving.
How services can work together in collaboration with the person with intellectual disability and their support network
Working collaboratively with people with intellectual disability
The guiding principles that underpin working with people with intellectual disability include a person-centred, recovery-oriented, and inclusive approach.
The person with intellectual disability should be the focus, with different members of their team working towards the person’s goals. In line with a recovery-oriented approach, people with intellectual disability should be seen as an expert in their own life, whilst professionals can share management knowledge. [3] See further information about the guiding principles.
Consider the following approaches when working with people with intellectual disability.
- It is important to spend time building rapport and trust; people with intellectual disability report that they find it easier to communicate with professionals if they feel comfortable and trust them. [1]
- Encourage active engagement and participation of the person in their care by:
- finding out about their communication, sensory and mobility needs and preferences in advance of appointments
- discussing their goals
- considering what will assist the person to actively engage in their care (e.g. provision of Easy Read information, appointments at their home, or at a time when public transport is readily available)
- determining their strengths and support structures e.g. friends, community groups.

- Assess the person’s capacity to understand information, make decisions, and provide informed consent. It is important to consider the following.
- Assess capacity to provide informed consent separately for each decision the person needs to make and at different stages as capacity can change.
- Facilitate supported decision-making to assist the person to make their own choices about their treatment and care as much as possible. [4] If a person is an involuntary patient in a mental health facility, still consider their preferences where possible.
- If a person requires a substitute decision-maker to make health care decisions on their behalf, they should still be i) provided with an explanation at each step in a way that they can understand and ii) be asked for their preferences where possible.
- For information on capacity to consent and supported decision-making in NSW, see the NSW Trustee & Guardian website which includes a Capacity Toolkit. There is also more information in 3DN’s Intellectual Disability Mental Health Core Competency Framework Toolkit (page 29). Also see 3DN’s Intellectual Disability Health Education course Consent, Decision-Making and Privacy – A Guide for Clinicians which is available for a small fee or free of charge for NSW Health professionals through My Health Learning on HETI.
- Engage the person in monitoring their treatment progress where possible.
Working collaboratively with support networks
Where appropriate, engage carers, family, and support workers as collaborative partners, considering the preferences of the person with intellectual disability, their level of intellectual disability and communication needs, and severity of their mental illness. It is important to recognise and value the knowledge held by the person’s support network.
Consider the following approaches when working with support networks.
- Intake and assessment – during this stage, with the person’s consent, support networks can:
- ask the person with intellectual disability what their preference is regarding the attendance of carers, family and support workers at appointments, and their level of involvement in the assessment (and treatment) process (e.g. attending for part or whole of the session)
- identify appropriate support persons at intake where possible. If the person does not have a support network, assist them to find an advocate, support worker or support person from a volunteer organisation if required
- convey the person’s communication preferences and assist the person they support and professionals to understand each other
- provide information on the person’s medical history and baseline functioning, and changes in mood and behaviours using collaboration tools such as the Wellbeing Record to chart baseline wellbeing and changes.
- share coping strategies that have worked in the past for the person and their strengths. Always check in with the person with intellectual disability to ask their thoughts on what their support networks have said.
- Treatment stage – during this stage, with the person’s consent, support networks can:
- be included in developing care plans (e.g. how they will help to monitor the person’s response to treatment including specific information to record, and when and how to seek help if required). Consider the support person’s knowledge and experience when discussing how they can be involved in the treatment and monitoring process.
- support the person to practise treatment strategies (e.g. through role plays) and use coping mechanisms at home (e.g. encouraging self-soothing, relaxation techniques)
- monitor the person’s progress (e.g. use a daily record of mood and behaviour, medication use and side effects, and use of coping strategies as appropriate). For example, they could complete a record such as Black Dog’s Daily Mood Chart on behalf of the person they support.
- identify early warning signs of declining mental health (discuss early warning signs, signs of a mental health crisis and steps to take with the support person)
- seek unscheduled follow-ups if necessary.
- Transfers of care – during this stage, with the person’s consent, support networks can:
- be included in planning for discharge or a transition
- continue to support treatment techniques and monitoring
- assist the person to seek additional support in the event of declining mental health or crisis.
Carers, family, and support workers emphasise the importance of providing regular written and oral feedback on the person’s progress. Where appropriate and with the person with intellectual disability’s consent:
- provide a summary to support networks after sessions (e.g. via email)
- arrange regular ‘check-in’ sessions, either in person, over the phone, or via teleconferencing.
For more information on working collaboratively with people with intellectual disability and their support networks, see the Mental health care pathway sections.
Working collaboratively with other services and agencies
Types of interagency working
- Multidisciplinary – when professionals provide support to the same person, but they have little contact with each other
- Interdisciplinary – professionals work separately conducting assessments and providing treatments, but meet to discuss the larger plan
- Transdisciplinary – a team of professionals who work together to undertake assessments, create care plans, and implement treatment strategies, often via one nominated primary service provider. [5]
The benefits and limitations of each interagency working approach are outlined in the following Table. [5] Whilst a transdisciplinary approach is not always practicable (especially for adults), an interdisciplinary approach can be considered where possible to utilise the experience of multiple professionals, provide co-ordinated care plans, and ensure that advice is not contradictory.
Benefits and limitations of different collaborative approaches
|
|
Benefits |
Limitations |
|---|---|---|
|
Multidisciplinary |
|
|
|
Interdisciplinary |
|
|
|
Transdisciplinary |
|
|
Many people with intellectual disability will receive care using a multidisciplinary approach. They may have little contact beyond sending reports to the person’s GP and occasional correspondence.
Collaborative approaches that can address the needs of people with intellectual disability, their support networks, and professionals
Support networks speak of the time and considerable stress of co-ordinating care across services for the person they support. This includes:
- finding suitable professionals
- providing information multiple times
- NDIS providers often require people to share information before their first appointment (the person may decide not to continue with the provider after this). After leaving a provider, information collected is protected by confidentiality laws; the person or their support network would need to request that information is transferred to any other provider or provide it themselves.
- relaying information, reports, and treatment plans between team members
- copying in other team members when communicating via email with health and disability services.
These and other common issues identified by people with intellectual disability, support networks and professionals can be mitigated by employing the following collaborative working approaches.
Connect and collaborate with local services and agencies to find out which professionals have experience working with people with intellectual disability to facilitate appropriate referrals. This can also identify any barriers that could impede referrals. Local specialist intellectual disability health teams and Statewide Intellectual Disability Mental Health Hubs, colleagues, people with intellectual disability and their support networks can assist with suggestions. New initiatives such as GROW for primary care providers in the Central and Eastern Sydney Primary Health Network can assist with service navigation (in addition to training and advocacy).
To help reduce this often-mentioned burden on people with intellectual disability and their support networks, take steps to implement the following practices.
- Identify and record details about the person’s existing supports and services.
- Gain consent to share history, assessment results and reports, whilst adhering to privacy legislation and local consent policies.
- Utilise joint or co-ordinated assessments, for example a joint assessment involving mental health and disability professionals could allow expertise to be shared, an enhanced understanding of the person’s baseline behaviour and subsequent changes, and the development of a shared care plan.
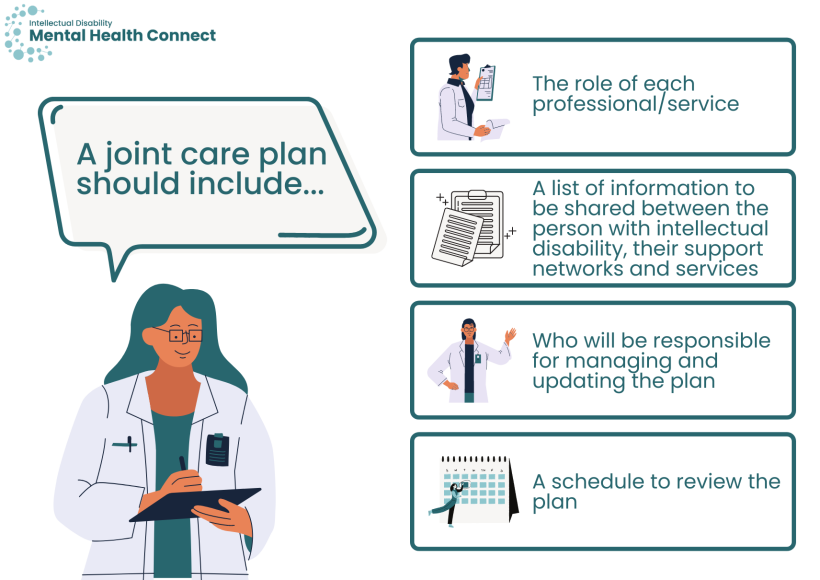
Joint care or treatment plans can ensure advice is complimentary and excessive demands are not placed on the person or their support networks. When developing a joint plan include:
- the role of each professional/service
- a list of information to be shared between the person with intellectual disability, their support networks, and services
- who will be responsible for managing and updating the plan (ideally one co-ordinator is assigned)
- a schedule to review the plan.
People with intellectual disability and their support networks often tell us that they would prefer their professionals to communicate more frequently around treatment planning and provide progress updates to the rest of the person’s team. The following processes can be utilised to support this (with the consent of the person or their substitute decision-maker where appropriate).

- Organise regular case conferences to review, plan, and co-ordinate care needs (the frequency reflects the person’s needs and circumstances) and keep all parties up to date with the outcomes.
- Informal ‘check in’ sessions can also be planned (e.g. every 10 sessions or every 3 months). It is important to note that additional meetings may come out of an individual’s NDIS funding budget and the benefits of a planning or check-in session versus a treatment session need to be considered.
- Email team members regular updates on progress and any changes in the care plan.
- Utilise online collaboration tools such as Teams or Google Drive to create a virtual collaborative space whereby professionals can provide regular updates (consider privacy and regulatory requirements).
People with intellectual disability are at risk of insufficient support after discharge from hospital, which can lead to declines in mental health and re-admission. In addition, they are at risk of a lack of consistent care and may subsequently cease contact with services during times of transition such as from child and adolescent to adult services.
- Plan early for any transfer of care between services at discharge or during a transition, working closely with other services.
- During any transition, appoint a care co-ordinator where possible, and ensure follow-up from the referring service.
For more detailed guidance see the Transfers of care section.
Collaboration also enables professional capacity building. Seek advice from professionals within and between sectors and from specialist tertiary intellectual disability mental health services where needed.
Professionals and services can also co-ordinate joint training and education initiatives that engage representatives from:
- different tiers of the mental health system (e.g. primary care, specialist services, inpatient services, tertiary services, and private practice) and
- different sectors (e.g. disability, health, justice, community and social services).
There are multiple ways to work collaboratively. Methods can be flexible and may include a combination of face-to-face meetings, phone calls, teleconferencing, reports, and email progress updates. Take into consideration the preferences of the person with intellectual disability and their support networks, their needs, professionals and services involved, geographic location of all parties, and their technical capacity when choosing methods.
What can help to facilitate partnerships and collaboration between services?
The following ideas can help professionals to connect with services and agencies to provide collaborative support to people with intellectual disability.
- Develop and share a directory of local services with professionals who have expertise or an interest in intellectual disability mental health (using methods similar to those suggested above for connecting with services).
- Engage and follow-up regularly with your local community mental health teams to discuss available services.
- Organise forums with service representatives in your local area network to identify agencies to collaborate with and refer to and address issues of concern and localised barriers. Identify any communities of practice or professionals who are ‘intellectual disability champions’ in your area from your directory who could help to organise and promote such an event.
- Provide education and training for staff on facilitating co-ordination across services and why this is important. You can provide professionals in your service with a link to this section to start and the tools described below. 3DN’s Intellectual Disability Health Education also has a course available on Enhancing Interagency Working with Health Professionals that is aimed at disability professionals (available for a small fee or your organisation may have a subscription).
- Provide a clear route for feedback if barriers to service engagement are identified (for both your service and external services). For example, this may involve identifying a single point of contact who can address any issues.
- Organise consumer focus groups in your local area. The Council for Intellectual Disability can provide advice and focus group facilitation services.
Considerations for working with specific services
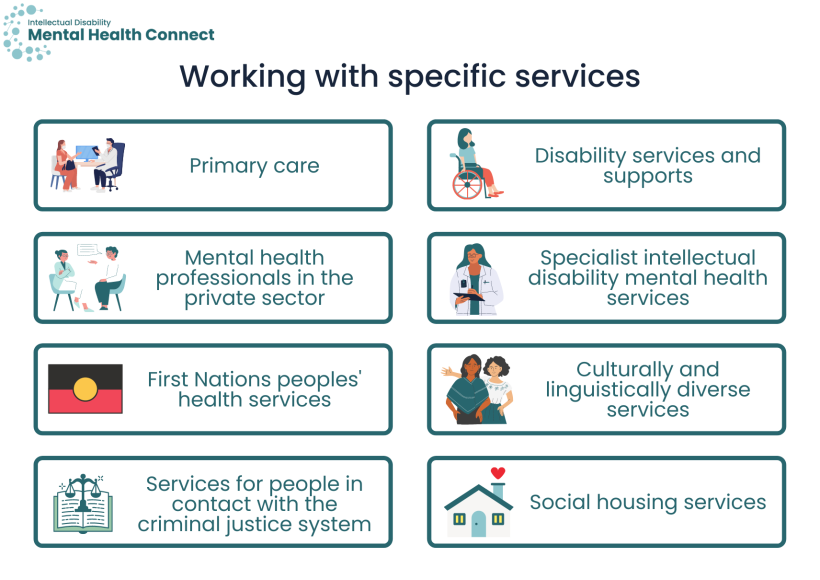
A wide range of health, disability and social services support people with intellectual disability. There are multiple benefits to working collaboratively with each service type. A key consideration for facilitating partnerships is to appreciate the differing perspectives of all stakeholders, recognise the unique knowledge and skills of each group, and utilise opportunities for mutual learning. An overview of key considerations for facilitating partnerships with each service type is provided below.
For more information on the roles of services, see the Role of health services, Role of disability services and Role of social services in a care pathway. For more information and links to the services below, see Services for mental health (within the people with intellectual disability section).
GPs have a key role at all stages of a mental health pathway and collaborate with the majority of mental health and support services to share information, plan care and provide support post-discharge. Considerations for working with primary care services and facilitating partnerships include:
- agreement with mental health services around roles in care planning, communication preferences for discussion and updates, and discharge planning
- development of connections with community-based mental health services to facilitate community-based treatment pathways (potentially reducing the need for emergency department and inpatient admissions)
- enhanced connections with disability support services such as respite.
Disability professionals provide a wide range of supports to people with intellectual disability including assistance in all areas of daily living from support workers, behavioural support strategies, and supported accommodation and employment. With the agreement of all parties, the attendance of support workers at mental health appointments and their ongoing collaboration can greatly support the assessment, treatment, and recovery process. They can also provide knowledge to other team members in a wide range of areas such as behavioural support strategies.
Considerations for working with disability services and facilitating partnerships include:
- clear goals and expectations of health and disability services including how each will be involved in care planning and management
- education and training for health professionals around working with disability supports, and for disability professionals around mental health (see 3DN’s Intellectual Disability Health Education courses for disability professionals)
- collaboration to provide community mental health and behaviour support pathways to reduce presentations to emergency departments, particularly from supported accommodation
- contact lists to assist identification of behaviour support practitioners if it is identified that a person would benefit from this support. Search for registered providers that offer behaviour support through the NDIS Provider finder tool.
- discussion around the development of behaviour support plans that can be used in inpatient mental health settings and how behaviour support practitioners may be able to provide support to health professionals around implementing plans
- developing pathways between local disability and social services in the provision of emergency respite. See Carer Gateway for more information.
- agreements on communication after referral to discuss employment options for a person with intellectual disability in more detail.
Private mental health professionals including psychiatrists and psychologists have an important role in supporting people with intellectual disability to receive supports in the local community, particularly NDIS participants.
Considerations for working with private mental health professionals and facilitating partnerships include:
- developing networks and supports for private mental health clinicians working with people with intellectual disability in the community
- agreements on care planning and case conferences, and communication preferences for discussions and updates with other members of the person’s team.
Specialist intellectual disability mental health teams can provide expert opinion and advice on assessment and treatment options including at points of transition.
Considerations for working with specialist intellectual disability mental health services and facilitating partnerships include:
- fostering connections between inpatient units and intellectual disability mental health teams to increase support available
- meetings and presentations by specialist services to mainstream mental health clinicians around how to access specialist services and supports available to increase awareness
- clear goals and expectations of each service involved including the specialist team (e.g. specialist teams generally do not take over primary responsibility for the person’s care; this will generally need to be provided by a psychiatrist or GP)
- working towards agreements on models of care, KPI definitions, data collection sources and methods.
See the Specialist intellectual disability mental health services page for more information.
Aboriginal Community Controlled Health Services, which include the provision of mental health care, and other First Nations peoples’ mental health providers, are vital to providing culturally safe support to First Nations peoples.
Considerations for working with First Nations peoples’ health services and facilitating partnerships include:
- developing contact lists and awareness of local (and state- or nation-wide) services that mainstream professionals can connect with
- agreements for collaboration, and how the person and their family and support network will be involved.
See the Working with diverse groups: First Nations peoples section for more information.
Collaborating with community CALD organisations can help to address language and cultural barriers to care. They can provide access to culturally appropriate support and cultural competency training.
Considerations for working with culturally and linguistically diverse services and facilitating partnerships include:
- increased links with local CALD mental health and disability organisations; Local Health District/Specialty Health Network CALD services can provide links to community CALD organisations
- gaining knowledge of interpreters experienced in working with people with intellectual disability
- increased provision of CALD resources to assist inpatient teams.
See the Working with diverse groups: Culturally and linguistically diverse people section for more information.
Services provided by Corrective Services NSW (e.g. Statewide Disability Services), the Justice Health and Forensic Mental Health Network, and organisations such as the Justice Advocacy Service provide specialised support from a person’s first contact with the criminal justice system to post-release from prison. They provide co-ordination of care to people who may be otherwise difficult to engage. Whilst mainstream mental health professionals generally do not provide services to people with intellectual disability while they are in prison or in remand, they have an important role post-release.
Considerations for working with services for people in contact with the criminal justice system and facilitating partnerships vary widely depending on the service type and circumstances of the individual, but include:
- collaboration with services for people in contact with the criminal justice system around protocols for information sharing
- protocols for linking in with people in custody before their release to facilitate continuity of care
- working with Corrective Services around opportunities for expert external clinician consultation for people with intellectual disability and mental illness or behaviours of concern
- working with Justice Health or Corrective Services on post-release rehabilitation and throughcare.
See the Working with diverse groups: People in contact with the justice system section for more information.
Housing services provide appropriate housing to meet the needs of people with intellectual disability with regular support.
Considerations for working with social housing services and facilitating partnerships include:
- forming connections with local public and social housing offices
- working with public housing offices to develop protocols to help people with intellectual disability with access to support for housing issues e.g. maintenance requests
- capacity building for social housing services around mental health and intellectual disability.
Tools to assist collaboration
Collaborative working plan with a person with intellectual disability
Developing a plan with the person with intellectual disability and their support network around how their team will work together can i) allow the person and their support networks to provide their input, ii) reduce uncertainty around how their services and supports will work together, and iii) reduce administrative burden for families and support networks.
This Working collaboratively with a person with intellectual disability and their team – Planning sheet template can be used to facilitate a discussion with the person with intellectual disability and their support networks as appropriate. There is also an Easy Read version that people can use to ask questions about how their team will work together and fill out.
The main sections of the planning sheet template include the:
- roles and responsibilities of services involved
- involvement of the person with intellectual disability, carers, family, and support workers
- collaboration options (e.g. joint assessments)
- communication methods and agreed upon schedule.
Collaboration protocols between services
Service managers and team leaders can identify or develop local collaboration protocols between services to facilitate effective information exchange and collaborative practices.
Services can develop Memorandums of Understanding (MoUs) to formalise their partnership and provide guidance as to how they will work together and communicate. MoUs are agreements between services or sectors at an overarching level, rather than about individual clients/patients.
When developing an MoU or other collaboration protocol consider:
- the need to be flexible and be mindful of administrative burden
- professionals from different service sectors can use different terms to talk about mental health support e.g. clients/consumers; behaviours of concern/challenging behaviours. Be aware of these differences and come to an agreement on preferred terms
- the benefit of consulting with professionals, people with intellectual disability and support networks in the development process.
An MoU template, Interagency collaboration to provide mental health care to people with intellectual disability – A Memorandum of Understanding (MoU) template, is provided that can be modified to meet the needs of services (opens a Word document). Collaboration protocols or MoUs can include the following.
- The aims and goals of the MoU, such as to facilitate interdisciplinary treatment to improve the mental health outcomes of people with intellectual disability
- Expertise of each service/agency
- Types of clients seen by the service and inclusion criteria
- The referral process, including capacity for urgent referrals (e.g. to mental health services from disability services and vice versa)
- Roles and responsibilities of each service including:
- how the services can work collaboratively (e.g. advice sharing, information sharing, case conferencing, joint assessments, joint care planning, transfer of care planning)
- services/supports each service will provide individually
- governance of each service.
- Communication processes for i) discussing the collaboration agreement and ii) care planning for people with intellectual disability. Include:
- potential methods of communication (e.g. telephone, video conferencing, in-person case conferences, reports) and
- guidance around frequency of contact for different situations.
- Information sharing process for e.g. clients’ medical history, assessment results, reports
- Consent procedures to follow for sharing information between services
- Maintaining confidentiality
- Procedures for resolving disputes and clinical stalemates
- Opportunities for capacity building between services
- Record keeping procedures relating to collaborative processes for clients, including how records can be shared if different systems are in place across services
- Monitoring the use of the MoU and procedures for review
- MoU timeframe
Resources
- Planning tools
- Working collaboratively with a person with intellectual disability and their team – Planning sheet template
- Easy Read version for people with intellectual disability – Working together with your mental health team
- Interagency collaboration to provide mental health care to people with intellectual disability – A Memorandum of Understanding (MoU) template
- Working collaboratively with a person with intellectual disability and their team – Planning sheet template
- 3DN’s Intellectual Disability Mental Health Core Competency Framework Manual – Section 5. Partnerships, Collaboration and Integration (page 26) and Intellectual Disability Mental Health Core Competency Framework Toolkit – Section 2.4 Involving support networks (page 21) and 2.5 Co-ordinating care across multidisciplinary services (page 23)
- 3DN’s Intellectual Disability Health Education course Enhancing Interagency Working with Health Professionals (aimed at disability professionals) and Consent, Decision-Making and Privacy – A Guide for Clinicians.
- 3DN’s Wellbeing Record can be used to chart baseline wellbeing and changes.
- NSW Trustee & Guardian website which includes a Capacity Toolkit – for information on capacity to consent and supported decision-making in NSW.
- Council for Intellectual Disability – can advise on inclusion and accessibility and can facilitate consumer focus groups.
- Weise J, Fisher KR, Whittle E, and Trollor JN. What Can the Experiences of People With an Intellectual Disability Tell Us About the Desirable Attributes of a Mental Health Professional? Journal of Mental Health Research in Intellectual Disabilities. 2018;11(3): 183-202.
- Evans E, Howlett S, Kremser T, Simpson J, Kayess R, and Trollor J. Service development for intellectual disability mental health: a human rights approach. Journal of Intellectual Disability Research. 2012;56(11): 1098-109.
- Australian Health Ministers' Advisory Council, A National Framework for Recovery-oriented Mental Health Services: Policy and Theory. 2013, Department of Health and Ageing: Canberra.
- Edwards P. Therapeutic Guidelines. Management guidelines: developmental disability. Version 3. 2012, Therapeutic Guidelines Limited: Melbourne.
- Moore T. Factsheet: Teamwork in early childhood intervention services: recommended practices (2015) [Retrieved 6th October 2021] from: https://www.speech-language-therapy.com/images/pdf/teamwork_in_early_child_intervention_services.pdf