Assessment
Jump to a section below
One of the first steps to getting help with mental health is an assessment. This is different from an intake session. During an assessment, mental health professionals will ask a range of questions about the person’s:
- current situation and life
- general health
- goals.
These questions will help the mental health professional to determine the most appropriate ways to help the person.
For people with intellectual disability, assessment may take more than one session.
What to bring
You or the person you support should be given a list of what to bring. The list may include:
- the referral letter from the GP
- results of any tests or assessments
- a list of medications
- information about the person’s communication preferences and their aids
- the person’s health folder or passport.
If you do not know what to bring it can be a good idea to contact the service and ask before the appointment.
How you can help
Create a folder of health information for the person
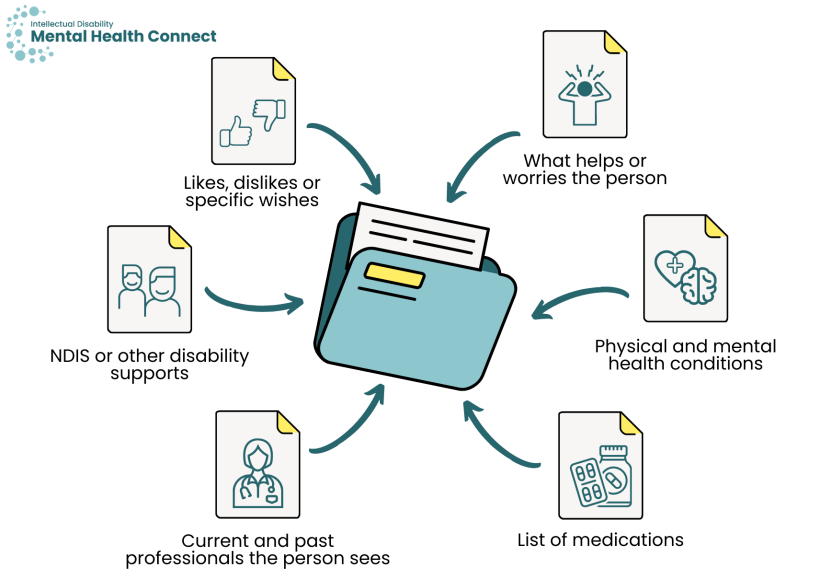
It can be hard to keep track of health information. Having a folder of health information may be useful. The person can bring this folder to all medical appointments. Sometimes, these folders are sometimes called health folders or health passports. The folder may include:
- physical and mental health conditions
- a list of medications
- current and past health and allied health professionals the person sees
- any NDIS or other disability supports
- likes, dislikes or specific wishes of the person
- what helps or worries the person.
There are resources available to help you do this. See 3DN's My Mental Health Passport that people can use to provide important information about their mental health to professionals. Another example is the Council for Intellectual Disability’s My Health Matters folder. You can find other information and examples, including the A2D Together Folder and Julian’s Key, here.
Ask the person’s GP or other health professionals if they can transfer information and history
If the person you support has had multiple assessments, it can be hard to answer the same questions many times. Many people and their support networks find it distressing to talk about stressful life experiences multiple times. If the person you support consents, you could talk to the person’s GP and other health professionals to see if they can transfer history and background information to the new health professional.
Questions during an assessment
The person you support will be asked a range of questions during an assessment. Questions may include:
- why they have come along today and the issues they would like help with
- if they have had mental health problems in the past
- if so, did they receive help? What worked and what did not work?
- whether they take any medication
- if they are seeing a psychiatrist, what current or past medications have they taken for mental health? Were there any side effects?
- what their life circumstances are, including friends, living situation, activities they like, work or study
- what their likes, dislikes and strengths are
- what their goals for recovery are, including what they would like to be able to do and what they want their life to look like. Recovery means getting better so the person can do the things they want to do.
How you can help
Prepare the person for the types of questions they may be asked
Prepare the person for the types of questions they may be asked and what their responses may be. Some people find it helpful to role play this before an appointment.
If the person you support tends to say “fine” when asked how they are feeling or just agrees or says “yes” to questions, talk to them about how they could let the mental health professional know about how they are really feeling. Let them know it is OK to speak up to get the help they need.
Help the person provide information
With the person’s consent, you could help provide information about the person’s baseline or normal functioning. This could include information about:
- what the person needed help with and what they did by themselves before symptoms started
- examples of things the person enjoyed
- whether changes in the person's mood, behaviour and functioning were sudden or more gradual, and when they began
- whether there were any changes in the person’s life.
You could also provide information on behaviours, including:
- behaviours that are usual for the person
- behaviours that are not usual for the person and when they started or increased in intensity
- what you think changes in behaviour might be signalling
- whether there are mental or physical health problems, environmental changes, communication needs or stressors that might be contributing.
Assessments in the emergency department (ED)
A doctor, who may be a psychiatrist, will assess the person you support. They may suggest some tests, such as blood tests. You should discuss any concerns the person may have with such tests.
After the assessment, the doctor will discuss options for care. It might be decided:
- it is safe for the person to return home
- The person should make an appointment to see their GP.
- If appropriate, a referral will be provided to a mental health professional at an outpatient clinic or community health service.
- If the person has attended the ED due to behaviours of concern, the doctor may suggest that the person’s behaviour support plan is reviewed, if they have one. If the person does not have a behaviour support plan, the doctor may suggest that they see a behaviour support practitioner to develop a plan. This is available through the NDIS.
- that the person needs to stay in hospital
- A Psychiatric Emergency Care Centre (PECC) offers short-term care to people who require urgent mental health care and intervention. A multidisciplinary team (a team of different professionals such as doctors, nurses and psychologists) will help the person and their support networks over a 24- to 72-hour period.
- The person may need to stay at an inpatient mental health unit at the hospital.
This Easy Read document has some questions you or the person you support can ask if they have to stay in hospital for their mental health.