Developing care pathways for people with intellectual disability
Jump to a section below
Key points
- The development of localised intellectual disability mental health care pathways can facilitate accessible, interconnected, and responsive services for people with intellectual disability.
- Care pathways include key actions and considerations as people with intellectual disability move through and between services including from referral to post-discharge.
- Benefits of care pathways include reduced workload through less duplication, improved communication, and improved working relationships. [1-3]
- Key considerations for developing a care pathway include planning and consultation with key stakeholders and developing care pathway content from mental health promotion to discharge and transitions of care.
- The implementation of care pathways includes education and training for clinicians in its use and an evaluation of outcomes.
Care pathways and their benefits
The development of localised intellectual disability mental health care pathways through and between services is an important step to improve access to mental health care for people with intellectual disability, help them navigate the mental health system, and improve mental health outcomes for this population. Care pathways can be defined as ‘a complex intervention for the mutual decision making and organisation of care processes for a well-defined group of patients during a well-defined period’ [4, 5] and also include ‘the ways different services interact with each other, and how people access and move between them’. [6]
A care pathway generally spans the whole health journey, including mental health promotion, from referral to post-discharge, and transitions between services. A care pathway is different to a clinical pathway that often refers to a specific short-term pathway in a clinic or hospital relating to a certain illness or procedure. [7] However, the terms ‘care’, ‘clinical’ and ‘service pathway’ are often used interchangeably.
In general, characteristics of care pathways include: [5]
- the facilitation of communication among team members and with the person and their supporters
- a statement of the goals and key elements of care based on evidence, best practice, and people’s characteristics and expectations
- the organisation of the care process by co-ordinating the roles and sequencing the activities of the multidisciplinary care team, the person, and their supporters
- the documentation, monitoring, and evaluation of variances and outcomes, and
- the identification of appropriate resources.
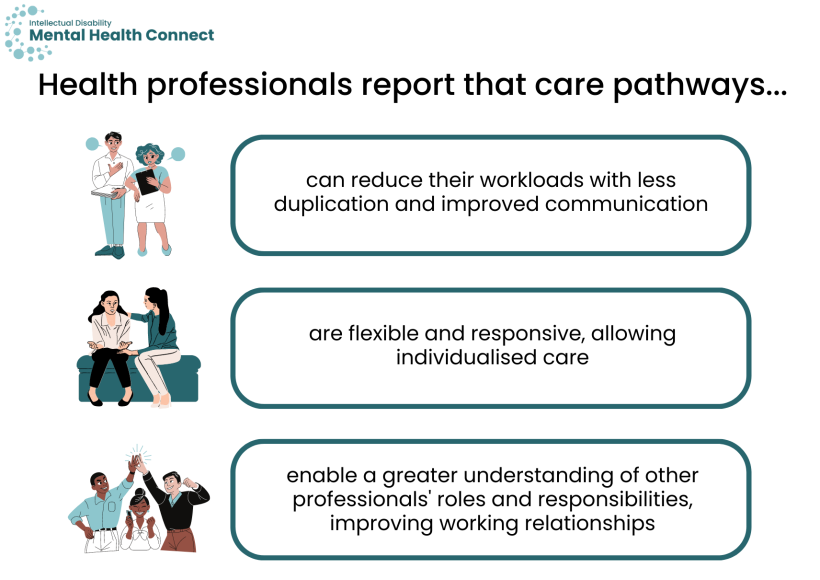
Health professionals report that care pathways:
- can reduce their workloads with less duplication and improved communication [1]
- are flexible and responsive, allowing individualised care [8]
- enable a greater understanding of other professionals’ roles and responsibilities, improving working relationships. [2, 3]
A care pathway-based approach in a specialist intellectual disability inpatient unit resulted in significantly shorter lengths of stay, and a subsequent three-fold increase in the number of admissions that could be accepted into the service. Working jointly with community teams ensured good continuity of care and timely discharges. [9]
Types of care pathways for people with intellectual disability
Depending on the type of service, care pathways can include a person with intellectual disability’s path:
- through a particular service, including mental health promotion and from referral to post-discharge
- between services within a hospital or Local Health District (LHD)/Specialty Health Network (SHN) such as acute care, inpatient, community mental health, allied health, rehabilitation, and specialist intellectual disability services
- between government and non-government services within the local community including:
- health (e.g. GPs, private psychiatrists and clinical psychologists, speech and language therapists, occupational therapists, physiotherapists)
- disability (e.g. behavioural support specialists, respite)
- social services (e.g. housing, education, and vocational supports)
- the community and voluntary sector (e.g. advocacy services, support groups, social and recreational groups).
Considerations for developing intellectual disability mental health care pathways
The process for developing localised intellectual disability care pathways varies widely depending on the service type, size, location, and place within the wider service sector.
The form of a care pathway will also vary, but could include guidance, checklists, diagrams illustrating the care pathway, flowcharts to assist with referral decisions and options, and service directories/maps.
The following considerations are broad and provided to assist service leads, managers, and clinicians to begin planning how they could develop a care pathway in their own service or district, and content it may include. Some guidance will be more applicable to certain service types than others.
The information in this section is also summarised in Development of localised intellectual disability mental health care pathways – A planning tool that services can use to initiate planning.
See 3DN’s The Guide – Accessible Mental Health Services for People with an Intellectual Disability that outlines best practices for making mental health services accessible for people with intellectual disability and further information about care pathways.
Planning
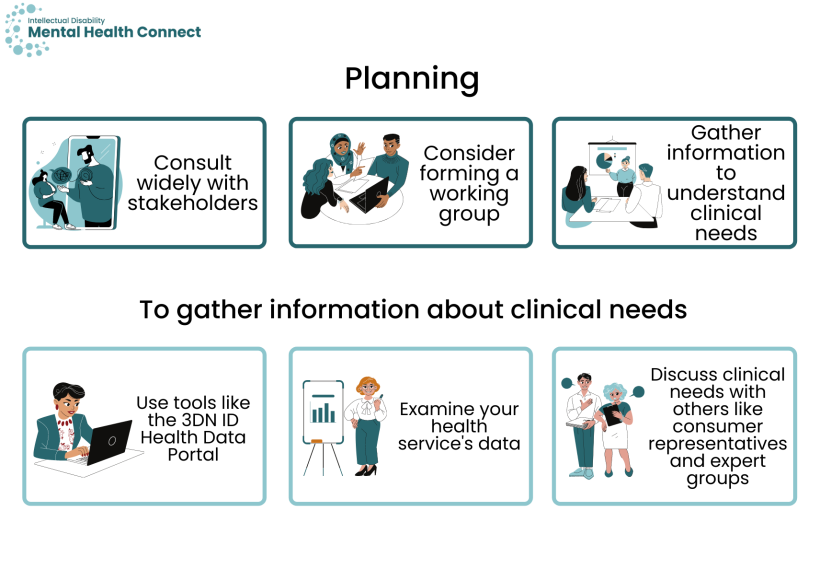
Joint planning is key to developing effective pathways.
- Consult widely with stakeholders, including with people with intellectual disability and their support networks (carers, family, paid and unpaid support workers), clinicians, managers, and government and non-government health, disability, and social services in your local district. Ask questions around support needs, experiences with local services and supports, gaps in services, and experiences navigating mental health and associated services.
- Consider forming a working group with representatives from all key stakeholder groups including people with intellectual disability and their support networks. Planning days or workshops can be effective at key stages of development.
- Gather information to understand the clinical needs of people with intellectual disability in the district.
- The 3DN Intellectual Disability Health Data Portal can be used to support LHDs and SHNs across NSW to understand and respond to the health needs of people with intellectual disability in their area. This interactive data portal uses results of the linkage of multiple service systems data to develop a regional profile of the demographics, health profile, and health service usage for people with intellectual disability. The Intellectual Disability Health Data Portal can be accessed following written approval from your Chief Executive.
- Examine your health service’s data (note, people with intellectual disability are usually not observable in administrative data as intellectual disability is poorly recognised and inconsistently coded).
- Discuss the clinical needs of people with intellectual disability with:
- consumer representatives within your health service
- consumer organisations locally or at a state or national level e.g. the Council for Intellectual Disability, Inclusion Australia, People with Disability Australia
- local disability service providers and peak disability service provider groups e.g. National Disability Services (NDS)
- expert groups e.g. intellectual disability health and mental health teams and clinical academic leads at e.g. 3DN or the Centre for Disability Studies (centres in other states include Monash Health’s Centre for Developmental Disability Health in Victoria and the Queensland Centre for Intellectual and Developmental Disability).
- Gather information about existing services for people with intellectual disability in your area. It is important to map i) what services are available and what information is known about them, ii) what information is not known about these services, and iii) what services are unavailable.
| Within own service | Outside of own service |
|---|---|
| Consult with different departments/professionals in mainstream services and determine which routinely see people with intellectual disability; if some do not, find out why. |
Create a directory or map of professionals and services with expertise in your local area through e.g. consultation with people with intellectual disability and their supporters, colleagues, PHNs, local Intellectual Disability Health Teams. For example:
Gather information about their:
See here for an example mental health service directory. Also map services that have the potential to work with people with intellectual disability. They may require support from others to do so such as via a tertiary intellectual disability mental health service or hub-and-spoke model. See this list of specialist intellectual disability mental health services and the Agency for Clinical Innovation’s information on specialised services on their intellectual disability health network resources and toolkit page. |
| Find professionals with expertise in your local services through e.g. colleague recommendations, the local Intellectual Disability Health Team | Seek out specialty streams and programs within your local PHN activities e.g. CESPHN GROW Service Navigators) |
| Determine specialised capacity locally or that may be accessible through outreach (e.g. Intellectual Disability Health and Mental Health Teams; Statewide Intellectual Disability Mental Health Outreach Service) |
Connect with NGOs with expertise |
| Start a register of professionals and knowledge/skills they can provide e.g. special skills around prescribing, physical health, behavioural or psychological management, interagency linkages, etc. | Form academic partnerships |
| Form linkages for capacity building within the NSW Ministry of Health or ACI |
- Identify whether existing inter-agency protocols/agreements exist to facilitate co-operative working practices and referrals. Local inter-agency protocols can clarify the roles of agencies and multidisciplinary staff, referral procedures, and opportunities for joint assessment and interventions. For more information on working collaboratively with other services and agencies see the Working with people with intellectual disability and their team section.
- Review evidence-based guidelines where available, for example:
- Developmental Disability guidelines from Therapeutic Guidelines (a subscription website), including managing psychiatric disorders in people with developmental disability.
- Prescribing guidelines for people with intellectual disability, Intellectual Disability Mental Health Core Competency Framework Toolkit, page 34.
- The Centre for Developmental Disability Health’s Healthcare for adults with intellectual disability Clinical Guideline and/or autism spectrum disorders: Clinical Guideline. Monash Health which includes information also relevant to mental health.
- NICE Guidelines from the UK
- Mental health problems in people with learning disabilities: prevention, assessment and management
- Care and support of people growing older with learning disabilities
- Challenging behaviour and learning disabilities: prevention and interventions for people with learning disabilities whose behaviour challenges
- General key considerations from the Care pathways for people with intellectual disability section can be included in a service’s pathway to guide clinicians and providers. Also see this section for the clinical aspects of each stage of a care pathway in addition to the Intellectual Disability Mental Health Core Competency Framework Manual and Toolkit.
- It is beneficial to develop an intellectual disability mental health resource folder on your service’s intranet or in a shared drive that is readily accessible to clinicians, and highlight resources that are available in your care pathway.
Care pathway content
This section identifies key actions for services when developing each stage of a care pathway.
- Include and encourage the routine use of mental health promotion activities for people with intellectual disability specific to your service. For more information see the Mental health promotion section.
All services should be accessible to people with intellectual disability (see the Guiding principles section for national and international policies outlining the responsibilities of health services). Encourage clinicians to view the mental health of people with intellectual disability as core business of any mental health service. It is important to equip each component of your service with appropriate intake processes to ensure they are accessible for people with intellectual disability. Consider each of the following points and include information on accessible intake procedures for clinicians to consult in your care pathway.
Referral
- Develop accessible information about the service and treatments available for people with intellectual disability, their support networks (and disability service providers). See 3DN’s Making mental health information accessible for people with intellectual disability – A Toolkit and the Australian Government’s Easy Read Style Manual for more information on making information accessible. Include a list of available accessible information in the care pathway so clinicians know what is available.
- Consider whether referral criteria can be modified for people with intellectual disability accessing your service. For example, while a person with a mild to moderate anxiety disorder may not meet the inclusion criteria for a community mental health service, a person with intellectual disability with anxiety and complex needs may require the level of care provided by such a service.
- Develop the capacity for the referral of priority cases from other health or disability services. Develop guidelines around this and ensure clinicians are aware of these.
- Nominate an intellectual disability care co-ordinator who can co-ordinate access, referral, and intake for people with intellectual disability. Ensure clinicians are aware of who the co-ordinator is and what their role is.
Intake
- Assess whether the timeframe for intake will meet the needs of a person with intellectual disability.
- Create intake forms that include information to document for people with intellectual disability (e.g. communication aids, support networks, behaviour support plan). Include details on how clinicians can best utilise these. See the Council for Intellectual Disability’s My Health Matters and the A2D Together Folder, which summarise this information.
- Develop a clear set of steps to take if a person with intellectual disability is not suitable for your service (e.g. provide an alternative to the referrer and the individual).
- Compile information on referral processes to disability and health services in the area and develop partnerships with local services. Include clear referral criteria for all relevant services in the pathway.
- Develop resources for clinicians detailing available local and statewide specialised intellectual disability health and mental health services. If the service or LHD/SHN has an intellectual disability mental health team, consultant, or care co-ordinator (e.g. Clinical Nurse Consultant), outline their role, responsibilities, and advice they can offer the team.
- Include alternative consultation service contact details if additional advice is needed or no such role or team is available in the district (e.g. the children and young people and adult Statewide Intellectual Disability Mental Health Hubs). See more information on specialist intellectual disability mental health services here.
- Review whether your service’s standard mental health assessment and outcome measures are suitable for people with intellectual disability. Develop and disseminate a list of screening, assessment, and outcome tools to consider/be completed with people with intellectual disability. House the list in a readily accessible and well-defined intellectual disability mental health resource list on your intranet or shared drive for clinicians to access (see a list of assessment tools here).
- Specify any information specific to your service that clinicians need to document during the assessment stage (e.g. specific screening or assessment tool results; results of medical tests); create checklists/forms and document in the care pathway.
- Depending on links to other services in the hospital or district, include opportunities for multi-service assessments, and include the criteria and process for such assessments.
- Develop environmental and procedural considerations to meet people’s physical and sensory needs (such as accessible clinics for e.g. wheelchairs) and to reduce anxiety (such as setting up a quiet room for people to wait in before their appointment; arranging an informal pre-assessment visit if indicated). See practical considerations for consultations in 3DN’s Intellectual Disability Mental Health Core Competency Framework Toolkit, page 17. Also see Latrobe Community Health Service’s Improving accessibility and inclusivity of people with disability in a community and mainstream setting report for a broader discussion around improving accessibility.
- Research and include details of appropriate services/clinicians within your LHD/SHN or district that clinicians may require for referral during the assessment stage e.g.
- specialist intellectual disability mental health service
- specialist intellectual disability health service
- neuropsychologist or psychologist
- behaviour support specialist
- dietitian
- exercise physiologist
- speech pathologist
- occupational therapist
- special care dentistry service
- social worker
- Detail procedures if a service is deemed unsuitable for a person with intellectual disability during the assessment stage (e.g. an alternative suggestion to provide to the referrer, person with intellectual disability and their support networks).
- Outline steps a clinician can take if there is diagnostic ambiguity or disagreement (e.g. a clinician or service who can be consulted for advice).
- Discuss with your team and clearly list the roles and responsibilities of your multidisciplinary team with regard to providing care to people with intellectual disability including who is responsible for care co-ordination (if applicable). Encourage clinicians to clearly detail where this will differ for each person with intellectual disability.
- When developing care pathways for emergency departments, include clear guidance clinicians can consult when making admission decisions for a person with intellectual disability including available alternative treatment pathways in the community to prevent admission to inpatient units (where clinically indicated).
- Within your care pathway, include links to resources available on your intranet/shared drive or online that clinicians can utilise during the treatment stage that are specific to your service’s needs (e.g. prescribing guidelines for people with intellectual disability, modifying CBT techniques). See the Care pathways for people with intellectual disability – Treatment section for more information.
- At a service level, consult with clinicians, people with intellectual disability and their support networks as to how support networks can be involved in the treatment and monitoring process. Develop guidance for clinicians and reference this in your care pathway.
- Provide links to service directories/maps clinicians can consult when they need to refer a person with intellectual disability to i) a different tier of care within their service (e.g. suitable inpatient units) or ii) external services in the local area.
- Develop a list of contacts clinicians can consult when they require specialist treatment advice including local intellectual disability mental health and health teams, consultants, care co-ordinators and the Statewide Intellectual Disability Mental Health Hubs. Provide guidance around the circumstances in which to seek advice. Actively disseminate this list to clinicians and house it in your resource folder.
- Develop protocols for measuring treatment outcomes for people with intellectual disability. This may include the use of assessment tools designed for use with people with intellectual disability and brief questions for people with intellectual disability and their support networks around treatment satisfaction. Review data collected and implement changes as necessary.
- Develop protocols specific to your service that detail steps for discharge planning with a person with intellectual disability and their support networks including information to be included in transfer of care plans. Encourage clinicians to use our Planning for the discharge of a person with intellectual disability after a mental health admission – A planning tool by including a link in your care pathway.
- Consult with intellectual disability care co-ordinators, teams, and specialists to determine pathways to appropriate services for people with intellectual disability on discharge from acute care and inpatient services, including community mental health services and outpatient clinics. Detail options in the care pathway for clinicians to refer to. Also include options such as the Pathways to Community Living initiative which may be appropriate for people with severe and persistent mental illness who are at risk of a long inpatient-stay.
- Create a checklist of actions specific to your service for clinicians to refer to when following up with people with intellectual disability post-discharge and establish procedures to monitor this.
- Develop procedures for co-ordinating effective transfers of care between your service and others at key transition stages (e.g. between child and adolescent, adult, and older adult services). For example, nominate a transitions co-ordinator. See the Care pathways for people with intellectual disability – Transfers of care section for more information on effective transitions. Detail these procedures in your care pathway for clinicians to refer to.
Implementation
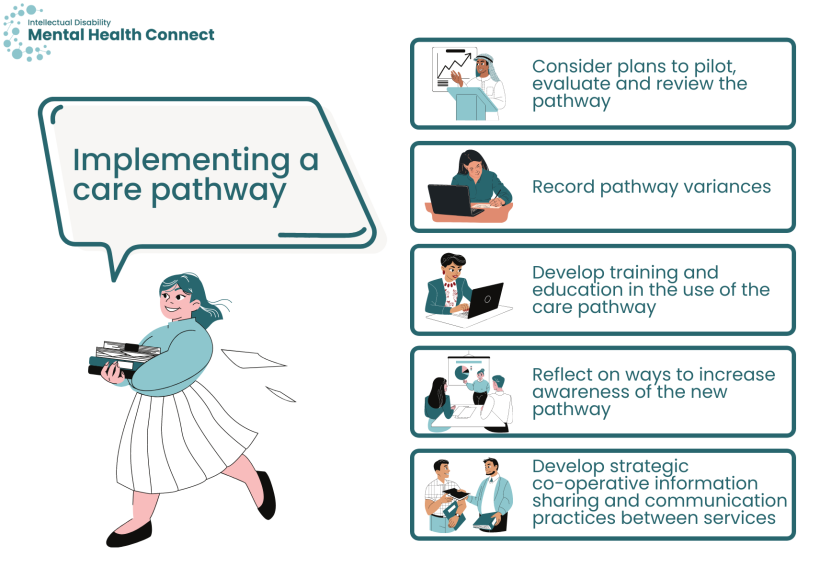
The implementation of a care pathway will vary depending on its scope. For all pathways, it is important to develop an evaluation plan so that it can be assessed against planned outcomes and refined as necessary.
- Consider plans to pilot, evaluate, and review the pathway. Evaluations include consultations with all key stakeholders including people with intellectual disability, their support networks, clinicians, and managers. See NSW Health’s Program evaluation resources page for more information.
- As part of a formative evaluation, record pathway variances (e.g. use of alternative assessment tools; referral to services not included in the pathway) to help inform the development of future versions. Develop ongoing monitoring processes relevant to your service.
- Develop training and education for clinicians in the use of the care pathway. This could include:
- the rationale for and benefits of the care pathway
- guidance around relevant clinical guidelines
- using case studies to guide clinicians through each step of the pathway
- providing an overview of appropriate services and supports in the local area or holding a networking session where possible
- training around communication skills when working with people with intellectual disability (see the Communication section)
- the use of screening and assessment tools
- how the pathway will be evaluated.
- Reflect on ways to increase awareness of the new pathway (e.g. discussion at clinical meetings, a presentation by a person with lived experience of intellectual disability on the benefits of a localised care pathway, or as part of a broader forum on intellectual disability mental health care).
- Develop strategic co-operative information sharing and communication practices between services included in the care pathway (within a hospital or LHD/SHN and with external services). See the Working with people with intellectual disability and their team section for more details.
Resources
- HealthPathways is an online manual used to help clinicians make assessment, management, and specialist request decisions for different conditions in a local context. Pathways are available for intellectual and developmental disability. For information about access see here.
- Clinical guidelines
- Developmental Disability guidelines from Therapeutic Guidelines (a subscription website), including managing psychiatric disorders in people with developmental disability.
- Prescribing guidelines for people with intellectual disability, Intellectual Disability Mental Health Core Competency Framework Toolkit, page 34.
- The Centre for Developmental Disability Health’s Healthcare for adults with intellectual disability Clinical Guideline and/or autism spectrum disorders: Clinical Guideline, Monash Health which includes information also relevant to mental health.
- NICE Guidelines from the UK
- Mental health problems in people with learning disabilities: prevention, assessment, and management
- Care and support of people growing older with learning disabilities
- Challenging behaviour and learning disabilities: prevention and interventions for people with learning disabilities whose behaviour challenges
- The 3DN Intellectual Disability Health Data Portal can be used to support LHDs and SHNs across NSW to understand and respond to the health needs of people with intellectual disability in their area. The Intellectual Disability Health Data Portal can be accessed following written approval from your Chief Executive.
- Making information accessible
- Roy A, Dunn L, and Bissaker S, Care Pathway for Young People and Adults with Learning Disability Who may have a Hearing Impairment. Implementation Guide. 2003, Birmingham and Black Country Strategic Health Authority: Birmingham, UK.
- Ahmad F, Roy A, Brady S, Belgeonne S, Dunn L, and Pitts J. Care pathway initiative for people with intellectual disabilities: impact evaluation. Journal of Nursing Management. 2007;15(7): 700-2.
- Simkiss DE. Integrated Care Pathway to Promote the Health of Looked after Children. Journal of Integrated Care Pathways. 2005;9(3): 123-8.
- Vanhaecht K, The impact of clinical pathways on the organisation of care processes. 2007, KU Leuven: Belgium.
- European Pathways Association. About care pathways E-P-A Definition of care pathway. Available from: http://e-p-a.org/care-pathways/ [28 September 2020].
- NICE. NICE Pathways – Mental health problems in people with learning disabilities. Available from: https://pathways.nice.org.uk/pathways/mental-health-problems-in-people-with-learning-disabilities [20 October 2020].
- Schrijvers G, van Hoorn A, and Huiskes N. The Care Pathway Concept: concepts and theories: an introduction. International Journal of Integrated Care. 2012;12(6).
- Hall J. A qualitative survey of staff responses to an integrated care pathway pilot study in a mental healthcare setting. NT Research. 2001;6(3): 696-705.
- Devapriam J, Alexander R, Gumber R, Pither J, and Gangadharan S. Impact of care pathway-based approach on outcomes in a specialist intellectual disability inpatient unit. Journal of Intellectual Disabilities. 2014;18(3): 211-20.