First appointment
Jump to a section below
Going to a GP to talk about mental health
You may already have experience going to the GP with the person you support. Going to the GP to talk about mental health will involve doing many of the same things.
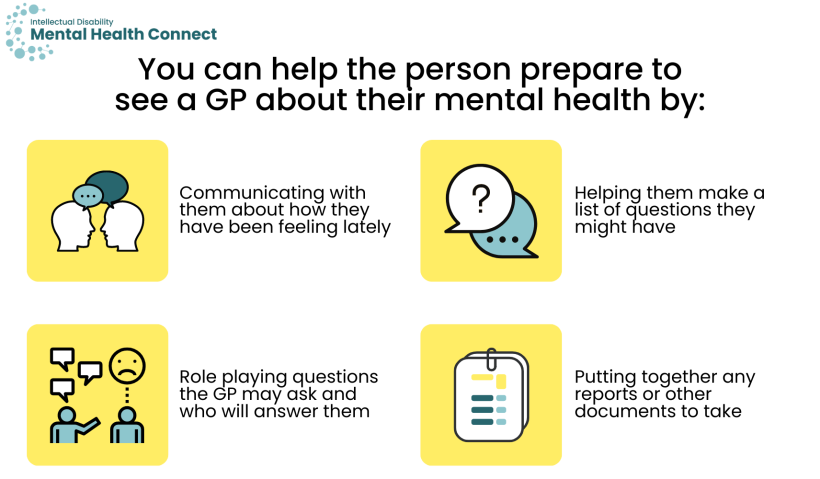
Before going to the GP to talk about mental health, you can help the person prepare by:
- communicating with them about how they have been feeling lately and noting this down
- helping them to make a list of questions they might have (e.g. what are their treatment options?)
- role playing questions the GP may ask and how they will answer them
- putting together any reports or other documents to take. You could use resources like the Council for Intellectual Disability’s My Health Matters folder to help put together information.
The GP will discuss options that could help. They may:
- give information on things the person can do to help their mental health (e.g. lifestyle changes, exercise, healthy eating), and how you can support them in this
- suggest whether medication may be an option, including the risks and benefits of medication and how a new medication would be trialled
- suggest a Mental Health Treatment Plan. People who have been diagnosed with a mental health disorder by a doctor can get subsidised sessions of psychological support through Medicare. You can find more information here.
- refer the person you support to a mental health professional (e.g. psychologist or psychiatrist). For more information on mental health professionals see the Mental health services section.
There is more information about seeing a GP about mental health here.
What happens when you first contact a mental health service?
The person’s GP may have referred them to a psychiatrist, psychologist or other health professional, such as an occupational therapist.
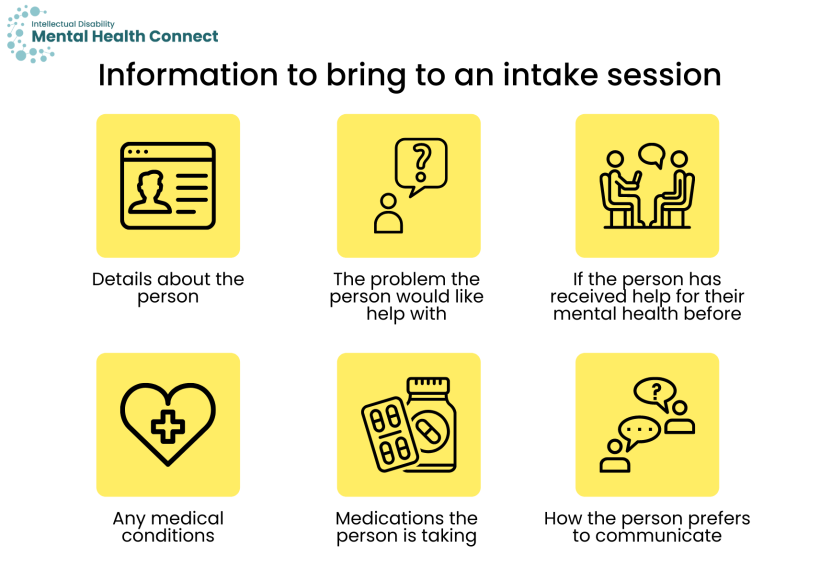
Before they start seeing a health professional, especially a psychologist, they may have what is called an ‘intake’ session. This may be done over the phone or in person. The intake session is to find out more about the person, the issues they are seeking help for, and whether the health professional or service will be right for them. They may ask:
- details about the person, such as their address
- what is the problem the person would like help with
- if the person has received help for their mental health before and what has helped
- if the person has any medical conditions
- if the person is taking any medications
- how the person prefers to communicate.
Some services may only seek information from the referrer during the intake stage. In this case, the person you support would have their first contact with the service when they start their assessment.
At the end of the intake session, they may make an appointment for an assessment. The health professional may also need to discuss with colleagues whether the service will be right for the person you support. Many people may be turned away after the intake session. It is important not to become discouraged. You can ask the service to suggest another health professional or service or go back to the GP for a referral to another service.
How you can help during intake
Prepare the person
- Talk with the person about the types of questions that the mental health professional may ask and what their responses may be.
- Discuss with the person what they would like you to tell the mental health professional if you or another supporter will go with them to the session or speak on their behalf during a phone session.
Provide information, with the person’s consent
- Provide background information, such as information about the person’s regular routines and behaviour and when any changes started occurring.
- Share any relevant assessment results, behaviour support plans, or prior mental health plans.
Find out about how the service can meet the person’s needs
- Find out about how the professional or service can meet the needs of the person. For example, do they offer home visits, or do sessions online if the person has trouble getting to appointments.
- If the person you support feels anxious in the waiting room, you could wait outside or in the car with the person and ask the receptionist to call you when the professional is ready.
If the person you support must go to the emergency department (ED) for their mental health
Upon arriving at the ED, a nurse will speak to the person you support. The person you support will speak to a doctor, but they may have to wait for some time before the doctor sees them. They may speak to a doctor who knows more about mental health such as a psychiatrist or trainee psychiatrist.
The ED can be a stressful experience. You can ask the nurse if there is somewhere quiet you can sit. Some EDs have sensory rooms or quiet spaces.
If the person lives in a group home or supported independent living
If the person lives in a group home or supported independent living, a support worker will likely need to accompany them to the ED. They can prepare by ensuring they have the following information available:
- the person’s person responsible or guardian
- the person’s communication preferences and aids
- the person’s health folders
- the person’s prescribed medications (e.g. tablets, injections, creams, inhalers, etc.) and any non-prescribed medications (e.g. vitamins)
- the person’s medical conditions
- any mental health professionals the person is currently seeing
- the person’s behaviour support plan, if applicable.
If they do not have information on the points above, they should bring the contact details of carers or family members whom ED staff can contact.
