Intake
Jump to a section below
Key points
- Ask the person or their support network how they wish to communicate.
- Include the person’s support networks where appropriate.
- Utilise existing intake/assessment information where available and appropriate to avoid multiple re-assessment.
- Consider that behavioural changes may signal mental ill health (or physical ill health).
- If a service is not suitable for a person, suggest alternative options.
This section provides key information around working with people with intellectual disability during intake or triage.
Intake processes differ for each service (e.g. in person, over the phone, information provided by referrer), so the below actions and information are general considerations that can be tailored to your service’s intake/triage procedures. Considerations for specific service types are provided at the end.
Below are key considerations and key questions you may have when working with people with intellectual disability during the intake stage.
For a list of specialist health services for people with intellectual disability see Specialist intellectual disability services.
Key considerations
Mental disorders can present differently in people with intellectual disability compared to the general population. Those with borderline and mild intellectual disability who can communicate their symptoms typically present in a manner familiar to most mental health professionals. People with more severe intellectual disability who have communication difficulties can present with atypical symptoms, often manifesting behaviourally. [1, 2]
- Be familiar with diagnostic overshadowing, whereby symptoms of mental ill health are misattributed to the intellectual disability rather than a manifestation of a mental disorder. [3]
- Assessment of potential underlying mental (or physical conditions) is important when an individual presents with behavioural changes or behaviours of concern. It is important not to assume they are merely due to the individual’s disability.
Below are some signs that could indicate depression or generalised anxiety disorder for a person with intellectual disability. While not a complete list of signs or mental health problems, it can provide some examples of how mental health problems can appear for people with intellectual disability.
Depression
Some signs that may indicate depression in a person with intellectual disability include:
- sad/flat facial expressions (e.g. less smiling, appears tearful)
- refusing to take part in normal activities or takes part but does not seem to enjoy them
- withdrawing from others (i.e. family, friends, and carers)
- physical problems (e.g. headaches, weight loss or gain, pain)
- anger (e.g. shouting, swearing, screaming, lashing out at others)
- refusing to eat meals, throws them away or spits out the food
- apparent decrease in skills
- seeking lots of reassurance that they are doing well or that they are a good person
Generalised Anxiety Disorder
Some signs that may indicate generalised anxiety disorder in a person with intellectual disability include:
- refusing to take part in activities or situations that may result in anxiety
- agitated or repetitive behaviours
- changes to expression or emotions (e.g. may seem more irritable)
- becoming more attached to carers
- physical problems (e.g. chest pain, stomach pain, nausea, headaches)
- asking for water or coughing as they have a dry mouth or difficulty swallowing
- easily fatigued
For more information on signs of mental illness in people with intellectual disability, 3DN’s Intellectual Disability Health Education has a free course called Specific Mental Illnesses – A Course for Carers.
During intake, find out about the person’s communication needs. This can include:
- asking the person with intellectual disability and/or support person how they prefer to communicate
- evaluating communication skills by asking some simple questions during a phone call or intake session e.g. name, age, address, and reason for referral.
For more information see the Communication section.
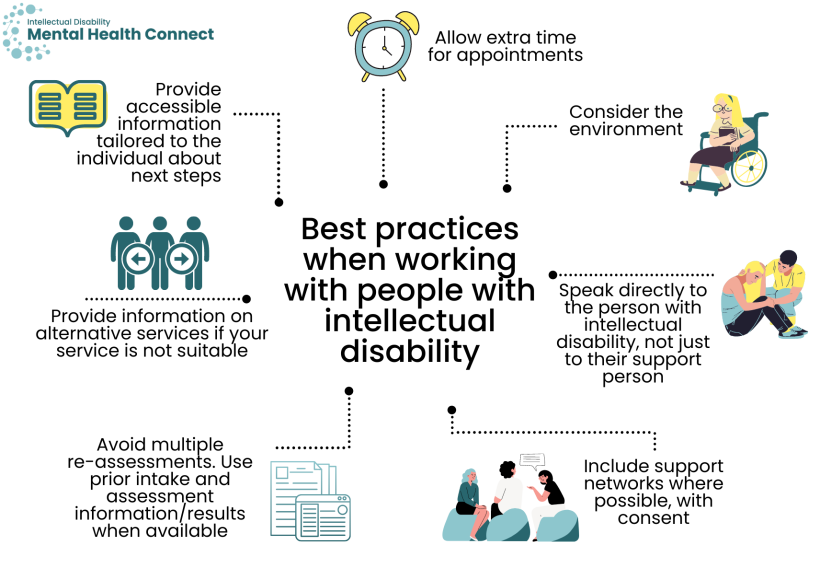
- Allow extra time for appointments.
- Consider the environment e.g. does the person have sensory needs that require a quiet space, do they require wheelchair access?
- Speak directly to the person with intellectual disability, not just to their support person.
- Include support networks where possible with consent of the individual.
- People with intellectual disability and their support networks speak of the need to avoid multiple re-assessments. Utilise prior intake and assessment information/results when available.
- If the service is not suitable for the person, inform them and their referrer and provide information on alternative services that may be appropriate.
- Provide accessible information tailored to the individual about the next steps e.g. Easy Read appointment confirmations. See 3DN’s Making mental health information accessible for people with intellectual disability – A Toolkit for more information.
See 3DN’s The Guide – Accessible Mental Health Services for People with an Intellectual Disability that outlines best practices in primary health care, public and private mental health services, and in specialised intellectual disability mental health services.
Provide details about your service to both:
- people with intellectual disability and their support networks via e.g. websites, Easy Read information sheets and contact with local GPs/disability services and
- health and disability professionals via e.g. websites, intranet, staff meetings.
Include:
- the role of your service and what it can offer
- details of professionals who are part of your service and what their roles are
- experience/interest in intellectual disability mental health of service professionals
- service referral criteria
- how to access the service/make an appointment.
Key questions
In addition to the presenting issues, general medical and psychosocial history, the following information is important to consider at intake for people with intellectual disability. Depending on your intake procedures, some of this information may be collected, or elaborated on, during the assessment stage.
- Cause of the individual’s intellectual disability
- Neurodevelopmental conditions
- Recent treatments/interventions and response
- Does the person have a history of non-adherence to medication?
- Behaviours of concern
- Including self-injurious behaviours, aggression, and self-neglect
- Risk of demonstrating inappropriate/sexual behaviour
- Have their behaviours led to exclusion from activities/community?
- Does the person have a behaviour support plan? When was this plan developed/last updated?
- Are restrictive practices used (including PRN medication)?
- Support needs
- Is the person an NDIS participant and what supports do they have in place?
- Support needs (e.g. personal care, household, Community Access, transport, meals)
- Do they attend respite?
- Daily activities e.g. paid or volunteer employment, day programs
- Details and contact information for individuals involved in the person’s care including:
- health professionals e.g. their specialty areas
- disability professionals and their role e.g. NDIS Support Coordinator, key worker, behaviour support practitioner
- team leader for those in supported accommodation.
- Decision making and informed consent
- Does the person usually make health decisions on their own, or do they have a person responsible who usually makes decisions and provides consent on their behalf? Do they have a Public Guardian?
- Collect details and contact information for their person responsible where applicable or person providing support around consent and decision making.
- Is the person able to provide informed consent for some/all decisions using supported decision-making?
- For information on capacity to consent and supported decision-making in NSW, see:
- the NSW Trustee & Guardian website which includes a Capacity Toolkit.
- 3DN’s Intellectual Disability Mental Health Core Competency Framework Toolkit (page 29)
- 3DN’s Intellectual Disability Health Education course Consent, Decision-Making and Privacy – A Guide for Clinicians. This course can be accessed for a small fee or is available for free through My Health Learning on HETI for NSW Health staff members.
- For information on capacity to consent and supported decision-making in NSW, see:
- If the person is in contact with the criminal justice system (see more information, see the section on working with People in contact with the justice system.
- Is the person homeless, or at risk of homelessness?
- Reports and documents to request
- Reports from specialists and other professionals e.g. occupational therapists
- Medication charts
- Neuropsychological assessments
- Behaviour support plan
When enquiring about information that has been collected, where possible, determine who it was collected by and when. This will help you to decide its relevance to the person’s current situation and if it remains accurate at the time of intake.
If assistance is required to determine the most appropriate supports for a person with intellectual disability, find services in the local area, or discuss a referral, advice can be sought from:
- Professionals who specialise in intellectual disability mental health (‘intellectual disability champions’) in your service district. To find specialists you can contact your Local Health District Specialist Intellectual Disability Health Team (see below), ask your colleagues and networks, or seek out presentations/workshops in this practice area.
- Intellectual disability health and mental health teams or staff in consultation roles such as Clinical Nurse Consultants.
- NSW Health funds six multidisciplinary Specialist Intellectual Disability Health Teams (SIDHT) in:
- Hunter New England Local Health District
- Northern Sydney Local Health District
- South Eastern Sydney Local Health District
- Sydney Local Health District
- South Western Sydney Local Health District
- Western NSW Local Health District
- Each of these teams provide outreach services to other Local Health Districts. For more information see the section around working with people in Rural and remote communities.
- NSW Health funds six multidisciplinary Specialist Intellectual Disability Health Teams (SIDHT) in:
- Statewide Intellectual Disability Mental Health Hubs
- The Hubs offer face-to-face and virtual care; specialised assessment, care planning, reporting and recommendations; and capacity building.
- For adults: Statewide Intellectual Disability Mental Health Outreach Service (SIDMHOS). Information is also available on the NSW Health website.
- SIDMHOS provides specialist advice to health professionals supporting an adult with intellectual disability where there are concerns about their mental health or behaviour. This includes individuals in contact with the criminal justice system.
- Referral is by an online form. To be eligible the person needs to have a diagnosis of intellectual disability (not borderline), and there needs to be a team around the person able to consider and implement any recommendations made. Ideally referrals are made, or supported, by public mental health services or private psychiatrists.
- The expectation is for referrers to have contacted any local specialist mental health services for adults with intellectual disability before referring to SIDMHOS. Potential referrers are encouraged to contact the service directly on 02 9767 7889 or [email protected] before completing the referral form.
- SIDMHOS is also available to provide training on mental health assessment and support for adults with intellectual disability.
- For children and adolescents under age 18: The Sydney Children’s Hospital Network Mental Health and Intellectual Disability Hub (SCHN MHID Hub). Information is also available on the NSW Health website.
- For the intake stage, both hubs provide advice on referral pathways or resources over the telephone.
- Please note advice and referral is only open to health professionals in NSW. Referrals for case reviews or joint team assessments are only offered to psychiatrists, paediatricians and LHD mental health services. Please see the Hub websites for more details.
- For adults: Statewide Intellectual Disability Mental Health Outreach Service (SIDMHOS). Information is also available on the NSW Health website.
- The Hubs offer face-to-face and virtual care; specialised assessment, care planning, reporting and recommendations; and capacity building.
Have details available of specialist services and professionals available and promote to staff in your service. Also consider coverage for after hours.
See more information on types of specialist intellectual disability services available.
For advice around clinical impasses at each stage of the care pathway see the Clinical stalemates section.
If it is determined that your service will not be suitable for the person, let them, their support networks and referrer know why. Suggest alternative appropriate services and support the person to access these services where appropriate. Reflect on whether capacity building in the area of intellectual disability or support from a specialist intellectual disability team could enable your service to take on such a referral in future.
If a referral you have made is not accepted, try to find out directly from the service why this was the case and whether the reason/s can be addressed. Stress the importance of the person with intellectual disability receiving access to care in a timely manner.
If the referral is still not accepted or the service is deemed unsuitable, ask the professional or service to suggest alternative options in the area.
Considerations for specific services
- Consider long or double appointments for people with intellectual disability.
- If seeing a person with intellectual disability for the first time, discuss with the person or their supporter whether a handover meeting with any past GP would be possible and beneficial.
- If you have limited experience providing care to people with intellectual disability, discuss considerations and approaches with colleagues or specialist services, especially for people with intellectual disability and complex needs. See the section on working with People with complex needs for more information.
- Also see the Assessment and diagnosis and Treatment sections for more information around providing care for people with intellectual disability within primary care.
- It is important that all people with intellectual disability have access to care from mainstream mental health services. Consider the intake criteria of your service to ensure it can accommodate people with intellectual disability.
- Consider whether intake criteria can be tailored for people with intellectual disability. For example, if a community service would not typically accept referrals for a mild – moderate anxiety or depressive disorder, consider accepting such a referral for a person with intellectual disability. They often have more complex psychosocial needs than the general population requiring a multidisciplinary approach.
- If your service has professionals with experience or expertise in this area, include these details when providing information about the service (e.g. on websites). Clearly indicate that people with intellectual disability can access the service.
- It is important to have flexibility in the amount of information that can be provided by the person at the time of referral. This may be less than the general population. Most people with intellectual disability will require a longitudinal assessment of their needs, with multiple contributors to provide input on their current situation.
- Also see the Transfers of care section for more information around providing care at discharge for people with intellectual disability within community mental health services.
- People with intellectual disability attend the emergency department at a higher rate than the general population, largely because of unmet physical and mental health needs. [4]
- People with intellectual disability may also attend due to escalating behaviours of concern. Behavioural changes may be due to a mental disorder or physical cause such as pain, constipation, urinary tract infection, toothache or earache. Be particularly aware of diagnostic overshadowing. See Why has a person’s behaviour changed? in the Assessment and diagnosis section for more information.
- Review any information the individual/their support person has brought with them. This may be a health folder or health passport such as My Health Matters or the A2D Together Folder. Also see 3DN’s My Mental Health Passport. Other examples of health passports can be found at the IDEAS website.
- If the individual has sensory issues, find somewhere quiet with low lighting where they can wait.
- Consider the person’s intellectual disability in triage decisions; people can experience high levels of anxiety in acute care settings which can be exacerbated the longer they have to wait.
- Determine whether a person from a culturally and linguistically diverse background needs a translator. As the individual may also have other communication needs, this is particularly important.
- 3DN’s Intellectual Disability Health Education has courses on emergency mental health care. These courses can be accessed for a small fee or are available for free through My Health Learning on HETI for NSW Health staff members.
- Also see the Assessment and diagnosis, Treatment, and Transfers of care sections for more information around providing care for people with intellectual disability in emergency departments.
- People with intellectual disability can find stays in psychiatric inpatient units very distressing. Consider whether there are any other viable options in the community.
- People with intellectual disability who live in supported accommodation may still require admission to psychiatric inpatient units; support workers cannot provide clinical care.
- On admission to a Psychiatric Emergency Care Centre (PECC) or psychiatric inpatient unit, consider the involvement of a local Clinical Nurse Consultant or specialist, a local intellectual disability mental health team or one of the Statewide Intellectual Disability Mental Health Hubs to provide advice around reducing the risk of presenting to an emergency department or requiring admission in future. See contact details for specialist intellectual disability services.
- Also see the Assessment and diagnosis and Treatment sections for more information around providing care for people with intellectual disability in inpatient settings.
Resources
- NSW Capacity to consent and Guardianship links
- Mental Health Act 2007
- Guardianship Act 1987
- NSW Trustee & Guardian – Public Guardian
- NSW Trustee & Guardian – Supported decision-making which includes a Capacity Toolkit
- NSW Civil & Administrative Tribunal – Guardianship and person responsible factsheet
- 3DN’s Intellectual Disability Mental Health Core Competency Framework Toolkit (page 29)
- 3DN's Intellectual Disability Health Education course Consent, Decision-Making and Privacy – A Guide for Clinicians.
- The Centre for Developmental Disability Studies developed the Health Care in People with Intellectual Disability: Guidelines for General Practitioners. These guidelines were designed to support general practitioners to provide comprehensive health care to people with intellectual disability.
- The Council for Intellectual Disability has checklists that help guide health professionals and administrative staff through reasonable adjustments they can offer before, during and after a health appointment to ensure they are accessible to people with intellectual disability. The checklists include links to Easy Read templates such as appointment letters and referrals.
- NSW Health’s Policy Directive Responding to Needs of People with Disability during Hospitalisation outlines the responsibilities for all staff working in hospitals who care for people with disability, including intellectual disability.
- 3DN’s Making mental health information accessible for people with intellectual disability – A Toolkit
- The Agency for Clinical Innovation (ACI) Intellectual Disability Network provides an Intellectual Disability Toolkit and series of videos designed to support health professionals understand the care needs of a person with intellectual disability.
- Resources for health professionals managing patients with intellectual disability (by CID for the Primary Care Enhancement Program) includes resources for health professionals to support the delivery of better care to people with intellectual disability, including a detailed Resources for Health Practitioners guide.
- Moss S, Emerson E, Bouras N, and Holland A. Mental disorders and problematic behaviours in people with intellectual disability: future directions for research. Journal of intellectual disability research : JIDR. 1997;41 ( Pt 6): 440-7.
- Fuller CG and Sabatino DA. Diagnosis and treatment considerations with comorbid developmentally disabled populations. Journal of clinical psychology. 1998;54(1): 1-10.
- Mason J and Scior K. ‘Diagnostic Overshadowing’ Amongst Clinicians Working with People with Intellectual Disabilities in the UK. Journal of Applied Research in Intellectual Disabilities. 2004;17(2): 85-90.
- Merrifield J. Meeting the needs of people with a learning disability in the emergency department. International Emergency Nursing. 2011;19(3): 146-151.