Role of health services
Jump to a section below
Key points
- Health professionals and services have a role in supporting a person with intellectual disability’s mental health.
- At all stages of a person’s mental health journey, they may benefit from allied health services (e.g. occupational therapist, speech pathologist) and support for physical health concerns, including dentistry.
- Health professionals often see people with intellectual disability for reasons unrelated to their mental health but can notice signs that may indicate a mental health problem. It is important to be aware of what these signs are and know how to respond.
- Across the mental health pathway, health professionals play an important role in sharing information with other professionals (with the person’s consent), ensuring service provision is consistent with the mental health treatment strategies and approach used, and supporting the person’s recovery by supporting other aspects of their health.
Working with people with intellectual disability when they are referred to you
A person with intellectual disability may be referred to a wide range of health and allied health professionals who can support their mental health journey, including dietitians and exercise physiologists.
All services can develop workforce capacity around working with people with intellectual disability and supporting them to have good mental health.
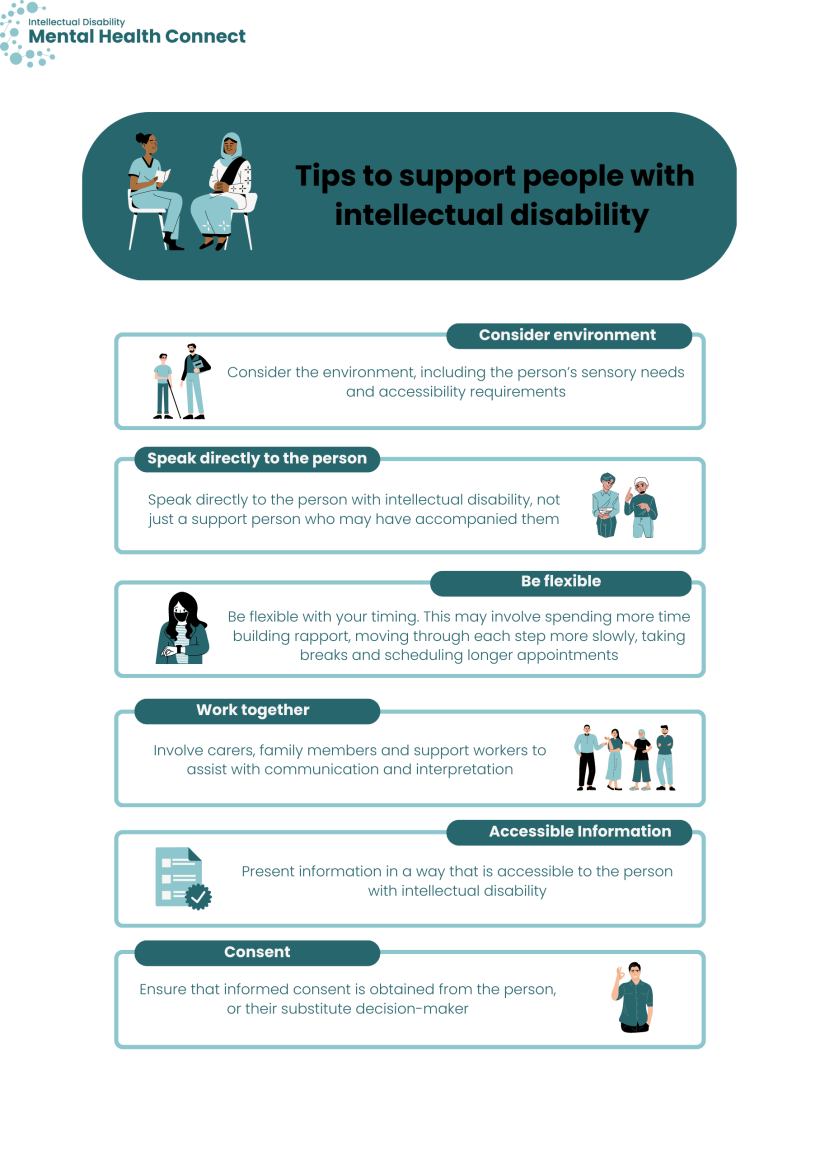
When working with people with intellectual disability, these tips may help you to support them:
- consider the environment, including the person’s sensory needs and accessibility requirements.
- speak directly to the person with intellectual disability, not just a support person who may have accompanied them. More information about communicating with a person with intellectual disability in health settings can be found here.
- be flexible with your timing. This may involve spending more time building rapport, moving through each step more slowly, taking breaks and scheduling longer appointments.
- involve carers, family members and support workers to assist with communication and interpretation. Support networks can also be involved in supporting and reinforcing treatments and strategies (e.g. exercise plans).
- present information in a way that is accessible to the person with intellectual disability. This may involve using Easy Read handouts, simplified visual guides, diagrams, visual cues, pictures, stories, and role playing to convey concepts. You can find out more about making information accessible in the Communication section and in 3DN’s Making mental health information accessible for people with intellectual disability – A Toolkit.
- ensure that informed consent is obtained from the person, or their substitute decision-maker. It is important to make every effort to ensure that the person can participate in decision-making as much as possible.
For more information about consent and decision-making, you may find 3DN’s Intellectual Disability Health Education course on consent, decision-making and privacy helpful. The course is available for a small fee, or can be accessed by NSW Health staff members for free through My Health Learning. Below are some links to information about capacity and guardianship in NSW that may be helpful:
- Mental Health Act 2007
- Guardianship Act 1987
- Office of the Public Guardian
- NSW Civil & Administrative Tribunal – Guardianship
Recognising mental health problems
Health professionals may be seeing a person with intellectual disability for reasons unrelated to mental health, but may notice signs of a mental health problem or the person may disclose they are having mental health problems. You can read more about recognising mental health problems here within the section for family and support persons.
To help recognise if a person with intellectual disability is experiencing mental health problems, you can:
- keep a record of information about a person’s usual health and wellbeing, and any changes that have been observed. Keeping a record can allow changes in a person’s health or mental wellbeing to be detected. You can find more information about how to record changes here with the person’s support networks and other health professionals. You could see if the person has a folder or health passport where this kind of information is collated
- be aware of diagnostic overshadowing, when signs of health or mental health problems are misattributed to the person’s intellectual disability
- investigate, or encourage investigation of behaviours of concern or any changes to the person’s behaviours, as these behaviours may be an attempt to communicate a physical or mental health problem
- investigate, or encourage investigation of unidentified pain or physical health problems that may be leading to distress or mental health problems, such as toothache, ear ache or urinary tract infection
- encourage the person to have regular appointments with their GP, so that there is proactive primary care to identify any mental health problems early
- communicate with the person about their mental health and assure them that they can come to you if they need help.
For information about how to help the person to seek support, see Overview of care pathways for people with intellectual disability.
Supporting someone at specific stages of the mental health care pathway
There are different stages in the person’s mental health care pathway where you could provide support. You can see an overview of the stages of the care pathway and what is involved in each stage here.
If you are involved in supporting the person to seek help for their mental health, you can:
- prepare the person for what to expect
- provide insights to the mental health professional about
- the best strategies to engage the person
- the best environment to engage the person
- any physical health considerations you are aware of as a health service provider that may affect engagement
- how to work with and engage the person’s support networks
- any relevant aspects of the person’s care plan and treatment
- encourage the person to write a list of questions to ask. See Your first appointment within the section for people with intellectual disability for more information and ideas. You could draw on the questions that you are asked as a health professional, or your experience working with the person, to help them prepare this list.
- The Council for Intellectual Disability has checklists that help guide health professionals and administrative staff through reasonable adjustments they can offer before, during and after a health appointment to ensure they are accessible to people with intellectual disability. The checklists include links to Easy Read templates such as appointment letters and referrals.
You can support assessment by helping to prepare the person for assessment in a similar way to how you might support the person at intake. You can prepare the person by discussing with them:
- what to expect, including what to take to the assessment. This could include any reports, plans or letters that you, as a health professional, may need to provide to support the assessment
- information to provide about their medical history, current medications and any recent assessments conducted
- factors that may influence the way the person engages with the assessment process.
Work with the mental health professional, as appropriate. This could be a phone call, teleconference or a joint assessment in some circumstances.
Encourage the mental health professional to liaise with the Statewide Intellectual Disability Mental Health Hubs if advice or a second opinion is needed.
Depending on your role, you can support the person during treatment planning and support the implementation of treatment strategies. If you would like to read about what treatment plans often include, you can find detailed information here.
You can support treatment planning by:
- ensuring that there is a single multidisciplinary treatment plan (if multiple treatment plans are unavoidable, share and check that they are not conflicting)
- sharing progress reports with others in the team and participating in regular multidisciplinary review sessions
- ensuring that you and all members of the team, including disability service, health and allied health professionals have a copy of the treatment plan.
You can support the implementation of treatment strategies by:
- monitoring for side effects of medications and encouraging the person to seek a medication review if things are not working
- encouraging GPs and psychiatrists to carefully consider the prescribing of psychotropic medications. For more information on responsible prescribing, see the Treatment page
- supporting psychological therapies by becoming familiar with the approach being taken and ensuring that your service provision is consistent with the approach
- supporting the person to engage in healthy lifestyle behaviours. 3DN’s Intellectual Disability Health Education has a free e-learning course on adapting healthy lifestyle interventions for people with intellectual disability that provides more information
- encouraging the person to have regular appointments with their GP and/or other health professionals, as good physical health can contribute to good mental health and recovery.
There are many things you can do to support the person’s transfer of care. You could:
- assist the person to implement their Transfer of Care plan, where appropriate, and know what specific role you play in the plan
- determine if there is a crisis plan in place and contribute to discussions around whether an emergency department management plan is required
- engage the person in healthy lifestyle interventions and behaviours relevant to your professional role
- encourage the person to follow-up with their GP, psychiatrist, or other mental health professional
- let the person know that it is OK to communicate with you if they begin to feel unwell again.
Supporting someone to have good mental health by supporting them to have good physical health
Physical and mental health have an impact on each other. By supporting someone’s physical health, you are also supporting them to have good mental health.
Depending on your role, you could also support good mental health in the following ways:
- encourage the person to eat a good and balanced diet
- encourage the person to engage in exercise and physical activity, making adjustments to the activities and environment to meet their needs, if needed
- investigate potential causes of poor sleep
- engage the person in preventative health checks and promote good preventative health measures
- ensure participation in healthy lifestyle activities and behaviours by adjusting practice to meet needs.
Resources for health professionals managing patients with intellectual disability (produced by CID for the Primary Care Enhancement Program) includes resources for health professionals to support the delivery of better care to people with intellectual disability, including a detailed Resources for Health Practitioners guide.
3DN’s Intellectual Disability Health Education has courses that can help expand your knowledge on topics such as:
- Adapting Healthy Lifestyle Interventions for People with Intellectual Disability (free to access)
- Cardiometabolic Health in People with Intellectual Disability (available for a small fee).
Find out more about mental health promotion here.