Accessible services
Jump to a section below
Key points
- There are individual, organisational, and service system level barriers to people with intellectual disability accessing mental health care.
- Professionals and services can work to provide accessible services by:
- providing accessible information about their service
- reviewing service intake criteria
- creating localised referral and care pathways
- creating interagency partnerships
- improving workforce capacity in intellectual disability mental health.
There are multiple barriers to mental health care for people with intellectual disability. These include:
- inconsistent eligibility criteria of services
- unclear referral pathways between services
- siloing of health and disability services (often making it difficult for people with intellectual disability and mental ill health to receive support from either type of service or move between the two)
- lack of interagency communication
- not identifying mental health disorders when people with intellectual disability present to services
- lack of workforce capacity in intellectual disability mental health. [1]
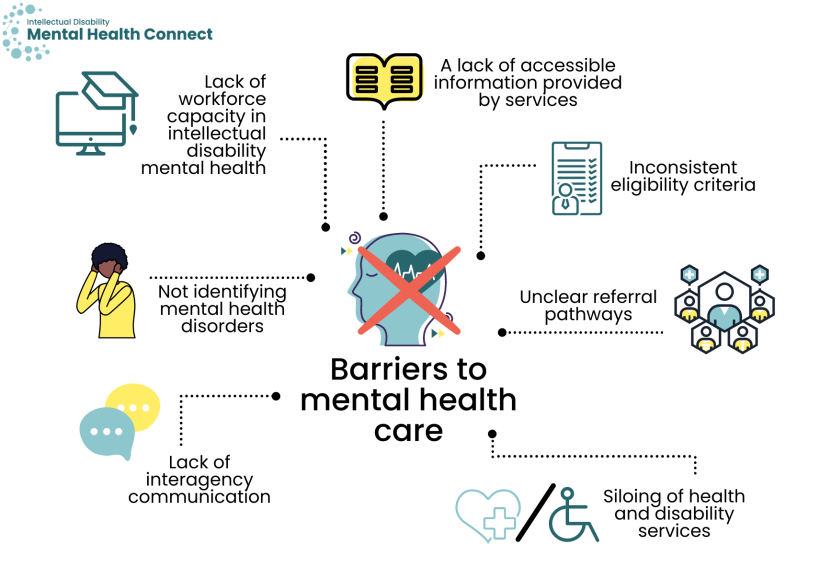
These are complex issues that occur at an individual, organisational, and service system level.
The following is an introduction to some of the practical steps you can take to help make your service accessible for people with intellectual disability and mental ill health. You will also find more information in The Guide: Accessible Mental Health Services for People with an Intellectual Disability.
Provide accessible information about what your service does and what it can offer
Accessible information is vital for people with intellectual disability to find and access support for their mental health. While accessibility needs differ for everyone, many people with intellectual disability can benefit from Easy Read information, which adapts standard information into a briefer copy and incorporates images to assist with comprehension. Many people also need to be actively supported to use Easy Read materials.
Make information accessible at all stages of a care pathway, including when providing details about your service.
Provide details about:
- the role of your service and what it can offer
- professionals’ experience and/or interest in intellectual disability mental health
- referral criteria
- how to access the service/make an appointment.
Ensure this information is available to both:
- people with intellectual disability and their support networks (e.g. via websites, Easy Read information sheets, contact with local GPs and disability services) and
- health and disability professionals (e.g. via your website, intranet, staff meetings).
You may like to view 3DN’s Making mental health information accessible for people with intellectual disability – A Toolkit for more details.
Review service intake criteria and accommodate people with intellectual disability
All people with intellectual disability have the right to receive care from mainstream mental health services. Similarly, people with mental ill health have a right to access services from disability providers.
If your service has any professionals with expertise or experience working with people with intellectual disability, include this in information about the service. Clearly indicate that people with intellectual disability can access the service.
Across Local Health Districts/Specialty Health Networks, endeavour to develop consistent eligibility criteria for people with intellectual disability. Consider whether intake criteria could be tailored for this population. For example, if a community mental health service would not typically accept referrals for a mild – moderate anxiety disorder, consider accepting such a referral for a person with intellectual disability. They can have more complex psychosocial needs than the general population necessitating a multidisciplinary team approach.
Consider a ‘no wrong door’ policy, which posits that people should receive appropriate treatment regardless of their entry point into the mental health system. If the service first accessed is not appropriate, it can still be a conduit to appropriate care through active referral and follow-up. This approach is commonly encouraged for people with co-occurring mental ill health and substance misuse problems but is also particularly suited for people with intellectual disability and co-occurring mental ill health. See the Comorbidity Guidelines website and No Wrong Door Initiative for more information.
Accommodating people with intellectual disability also includes:
- meeting people’s communication needs
- providing a physical environment that is accessible to people with intellectual disability and their support networks e.g. quiet rooms to meet sensory needs.
The Council for Intellectual Disability has checklists that help guide health professionals and administrative staff through reasonable adjustments they can offer before, during and after a health appointment to ensure they are accessible to people with intellectual disability. The checklists include links to Easy Read templates such as appointment letters and referrals.
Create localised referral and care pathways
There are a lack of localised referral and care pathways in NSW for people with intellectual disability and mental ill health. However, this is improving with the introduction of:
- NSW Health multidisciplinary Specialist Intellectual Disability Health Teams (SIDHT) in six Local Health Districts (Hunter New England, Northern Sydney, South Eastern Sydney, Sydney, South Western Sydney, and Western NSW LHDs).
- Staff such as Clinical Nurse Consultants can provide advice around referrals and pathways in your local area.
This website provides general information on intellectual disability mental health care pathways for mental health professionals and GPs and other health, disability and social service professionals. However, it is important for services to:
- tailor this information to your local area and service to create localised care pathways that are interconnected and responsive to the needs of people with intellectual disability. There is guidance in the Developing care pathways for people with intellectual disability section
- develop localised service maps/directories of professionals and services who can provide quality care to people with intellectual disability in your local area. For a list of services that people may require see the Services for mental health section (within the I am a person with intellectual disability section).
Work together
People with intellectual disability often have complex needs and require a multidisciplinary or interdisciplinary approach to care. Historically there has been siloing of health and disability services. Adults with intellectual disability and their support networks tell us that they rarely receive co-ordinated care. Many report that they would like their health and disability professionals to work more closely together. It is important that health, disability, and other services work together where possible to provide co-ordinated, consistent, and holistic care.
Developing local and regional partnerships between services and agencies can facilitate:
- co-ordinated approaches to care
- an understanding of the referral processes for i) health and ii) disability and related services
- exchange of knowledge between health, disability, and social service professionals.
There is further information on how you can achieve this in the Working with people with intellectual disability and their team section.
Improve workforce capacity
There is a lack of workforce capacity to provide quality mental health care to people with intellectual disability in Australia. Professionals report that they lack the knowledge, skills, and confidence in this practice area. [2] This is in part caused by a lack of undergraduate training for future doctors and nurses in Australia. [3, 4]
Seek and provide education and training opportunities for yourself and staff within your service or organisation. For example:
- The Statewide Intellectual Disability Mental Health Outreach Service (SIDMHOS) has an ECHO program that provides education and training sessions for registered health professionals in NSW via a weekly dial-in virtual training program.
- 3DN’s Intellectual Disability Health Education has courses to increase your knowledge, skills and confidence around intellectual disability health. There are courses for health professionals and disability professionals. There are also courses for carers, which are free to access. Other professionals such as those in social services will likely also find many courses useful. The majority of courses for health professionals can be accessed for free through My Health Learning on HETI for NSW Health staff members.
- The Council for Intellectual Disability provides training on making organisations accessible and developing Easy Read.
- Local communities of practice, in-services by ‘intellectual disability champions’ in your area, and webinars.
- Whittle EL, Fisher KR, Reppermund S, Lenroot R, and Trollor J. Barriers and Enablers to Accessing Mental Health Services for People With Intellectual Disability: A Scoping Review. Journal of Mental Health Research in Intellectual Disabilities. 2018;11(1): 69-102.
- Weise J and Trollor JN. Preparedness and training needs of an Australian public mental health workforce in intellectual disability mental health. Journal of Intellectual & Developmental Disability. 2018;43(4): 431-440.
- Trollor JN, Ruffell B, Tracy J, Torr JJ, Durvasula S, Iacono T, et al. Intellectual disability health content within medical curriculum: an audit of what our future doctors are taught. BMC Medical Education. 2016;16(1): 105.
- Trollor JN, Eagleson C, Turner B, Salomon C, Cashin A, Iacono T, et al. Intellectual disability health content within nursing curriculum: An audit of what our future nurses are taught. Nurse Educ Today. 2016;45: 72-9.