Treatment
Jump to a section below
Making a mental health care plan
After assessment, a mental health care plan is discussed. A care plan is a detailed plan with information about the person’s diagnosis, treatment options and any potential side effects. Care plans are sometimes also called treatment plans. Care planning should include the person you support, carers, family members, support workers and other relevant health professionals. The wishes and support needs of the person should be at the centre of all decisions about treatment.
Care plans should include information about:
- treatments and the mental health professionals who will provide them
- other health and disability services who will support treatment
- triggers that can affect mood
- signs that mental health may be declining
- who or what can help in different situations
- what to do in a crisis.

Carers, family members and support workers should have a copy of the plan.
Including all of this information in a plan is especially important for people who may live in group homes or supported independent living and may have multiple support workers. Regular reviews of this information should be scheduled. If changes to the person are noticed, support workers should contact the person’s next of kin or an appropriate medical professional.
There are also other things that can be included in a care plan to support mental health. These include:
- support groups and forums (either in person or online)
- having a healthy lifestyle (e.g. getting enough sleep, eating well and exercising)
- additional health or disability support services
- personalised emergency help card. An emergency help card can keep the person you support and others safe in a crisis. For more information go to the Emergency help card template.
Consenting to treatment
Either the person you support, or their guardian will need to provide consent for mental health treatment. The guardian may also be referred to as the ‘person responsible’. A person responsible is someone who can legally make decisions about the person you support’s health if they are unable to do so.
- Whether or not a person is able to make a decision about their health or treatment options can depend on the situation and the decision that needs to be made. This means that the person should be supported to be involved for every decision that needs to be made.
- It is important that our starting point is the assumption that the person has the capacity to make their own decisions, that we engage the person in decision-making to the fullest extent possible, and that we are meeting the person’s decision-making needs as we progress.
- You can support the person’s decision-making by making sure they can understand, consider and communicate their choices.
- If the person has a person responsible, they should be involved as appropriate.
How you can help
Facilitate decision-making
You may be involved in supporting the person to provide their own consent to treatment. You can make sure that the person is supported to make decisions about their treatment as much as possible.
Familiarise yourself with the care plan
It is important to be familiar with all aspects of the care plan so that you can respond quickly if you see signs that the person’s mental health may be declining. This includes knowing what to do in a crisis. For additional information on how to support a person in a mental health crisis, disability support workers may be interested in a course by 3DN’s Intellectual Disability Health Education on how to support a person in a mental health crisis. The course is available to access for a small fee.
Treatments that are available
There are many treatments that can improve mental health. Two of the main treatments are:
- psychological therapies (sometimes called ‘talking therapies’)
- medical treatments.
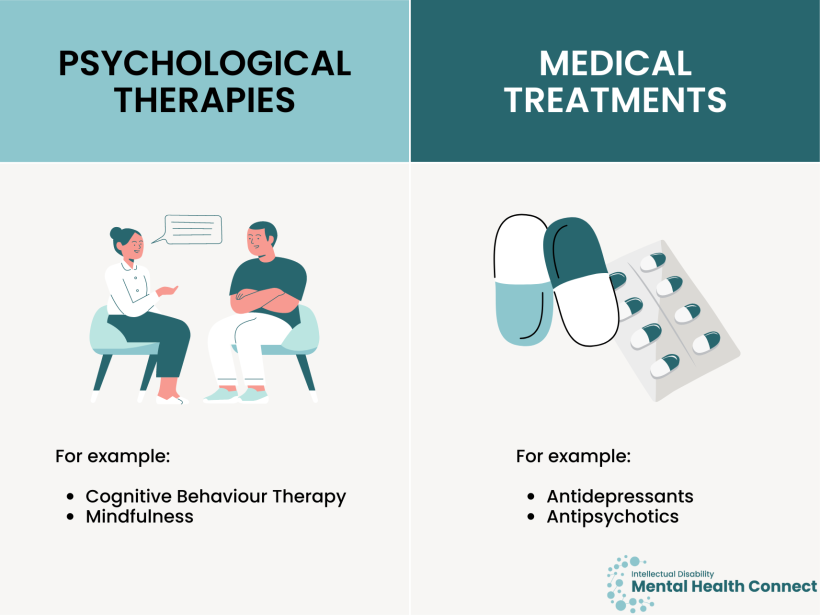
A combination of these treatments may be suggested.
It is important to see how the care plan works for the person you support. Often, the first treatment will not be the best one for them. If a treatment is not working, another one can be trialled.
Disability support workers can learn more about treatments and supports for mental illness in an e-learning course by 3DN’s Intellectual Disability Health Education. The course is available to access for a small fee.
Psychological therapies
Psychological therapy involves speaking to a mental health professional about thoughts, feelings and behaviours. It also involves learning tools to cope with stressors and strong emotions. Psychological therapies are usually provided by psychologists or counsellors.
Some of the common psychological therapies you may hear about are:
- Cognitive Behavioural Therapy (CBT), which can help people learn ways to change their thoughts and behaviours to have more positive feelings. You can find out more here.
- Mindfulness, which can help people to focus on what is happening now to calm their mind. You can find out more here.
Both CBT and mindfulness can be tailored for people with intellectual disability, depending on their needs and abilities.
Medical treatments
The person’s GP or psychiatrist may suggest medication for moderate to severe mental health illnesses. These medications are also known as psychotropics. Some types of mental illness, including bipolar disorder and psychosis, almost always require medication. You can find more information about types of medication for mental illness and side effects here.
Medication can also be prescribed for behaviours of concern that are severe and are not responding to other behavioural or cognitive therapies.
Psychotropic medication is often overused for people with intellectual disability, especially for those with behaviours of concern. People may be prescribed too high a dosage, for too long, and for the wrong reasons. There are things that doctors should carefully think about before prescribing medications to people with intellectual disability for mental illness or behaviours of concern. You could talk to the person’s doctor about these considerations and suggest they view the Treatment section of Care pathways for people with intellectual disability if they would like more information.
You may find the STOMP (Stopping over medication of people with a learning disability, autism, or both) resources from the United Kingdom useful. They have a medication pathway with information about ways you can make sure the person you support only takes the medication they need safely. Please note that these resources reference the UK’s National Health Service (NHS), and not all information will be applicable to Australian settings. There is also an Australian network, STOMPOZ.
How you can help
Join the person during their treatment sessions or appointments, if they agree
If the person agrees, it can be helpful to join them for at least part of their treatment sessions or appointments. By joining them, you can:
- help them understand information
- provide additional information where it is required. Support workers may also be able to provide a different perspective because they may support the person in other areas to their family members
- learn about psychological therapy plans. It is important that all supporters are familiar with psychological therapy plans so that care is consistent
- discuss how you can best support the person to use, for example, coping strategies between sessions, including specific terms for strategies that all members of the support network can use with the person.
Supporting and monitoring treatment
You can support and reinforce coping strategies at home and when out in the community. Mental health professionals can also help carers, family and support workers with techniques they can use if the person becomes distressed. Supporters can also assist with monitoring treatment progress. This could involve completing side effects or mood diaries that can be brought to review appointments. There is a feelings chart on page 48 of the Feeling Down: Looking After My Mental Health Easy Read guide. You could encourage the person you support to obtain a Home Medicines Review, where an accredited pharmacist will check that they are taking their medications correctly.
Support workers can keep a diary or log
For people who live in group homes or Supported Independent Living, it can be helpful for support workers to be aware of how the person’s mental health has been recently. This can help them with communicating the person’s needs and concerns at treatment sessions. It can be helpful to have a diary or log in which support workers can write brief notes after their shifts. Site managers should implement systems and support, so this information is up to date.
Provide help in other areas
The person may want help in other areas of their life. For example, they may want someone to help plan a healthy diet or exercise. Find out more about Other services. It is good if support workers in group homes or Supported Independent Living can have a list of supports in the local area available.
If the person you support must go to hospital for their mental health
People stay in hospital for their mental health when:
- it is not safe for them or others to be at home
- when they are being stabilised with new treatments.
If the person you support needs to stay in hospital for their mental health, they may be admitted as either:
- a voluntary patient – they have chosen to go to hospital and have a choice about when they leave. The statement of rights for voluntary patients can be found here (Easy Read information about these rights is here).
- an involuntary patient – a doctor has decided they must stay in hospital for their safety or the safety of others. It is not the person’s choice when they leave. The statement of rights for involuntary patients can be found here (Easy Read information about these rights is here).
Support while in hospital
Staying in hospital for mental health can be very stressful. There are many ways people with intellectual disability can get support, including:
- discussing with a staff member if they are worried or if someone or something is bothering them on the ward
- communicating with psychologists, counsellors or social workers in hospital if they need support
- communicating with an Official Visitor. Official Visitors are people who visit the hospital. They make sure people in hospital are treated well. Official Visitors do not work for the hospital.
You can discuss your level of involvement during the person’s inpatient stay with hospital staff such as the nurse unit manager.
Resources
- 3DN’s Intellectual Disability Health Education on how to support a person in a mental health crisis.
- Disability support workers can learn more about treatments and supports for mental illness.
- healthdirect has information on e.g.
- Support groups and forums e.g.
- Your Health in Mind has information about treatments and medication.
- NHS STOMP ‘Stopping over medication of people with a learning disability, autism or both’ resources. They also have a medication pathway. There is an Australian network, STOMPOZ.
- The statement of rights for voluntary patients can be found here (Easy Read information about these rights is here).
- The statement of rights for involuntary patients can be found here (Easy Read information about these rights is here).
- Information about the Official Visitors program in NSW.