Moving on from services
Jump to a section below
Discharge
Discharge usually refers to leaving hospital. It can also refer to the time someone finishes their planned sessions with a mental health professional, such as a psychologist.
Finishing with a mental health professional
It may be decided that the person you support no longer needs to go to regular sessions with a mental health professional, they have used all their subsidised Mental Health Treatment Plan sessions, or they no longer wish to continue. When this happens, a plan as to how the person can continue their recovery after regular sessions end will be discussed. This plan may include:
- tools and skills the person can continue using
- activities that could support good mental health (e.g. joining a support group)
- signs that the person’s mental health may be declining and what to do
- how support networks can continue to support recovery
- information that they need from that health professional that may be useful if further treatment is required in the future.
The mental health professional will usually plan to have follow-up sessions to check in with the person (e.g. after one month).
Leaving hospital
During the person’s stay in hospital, their mental health team should start planning what support they will need at discharge. This is called a Transfer of Care plan, or Discharge plan. The plan should be discussed with the person you support and carers, family members and support workers.
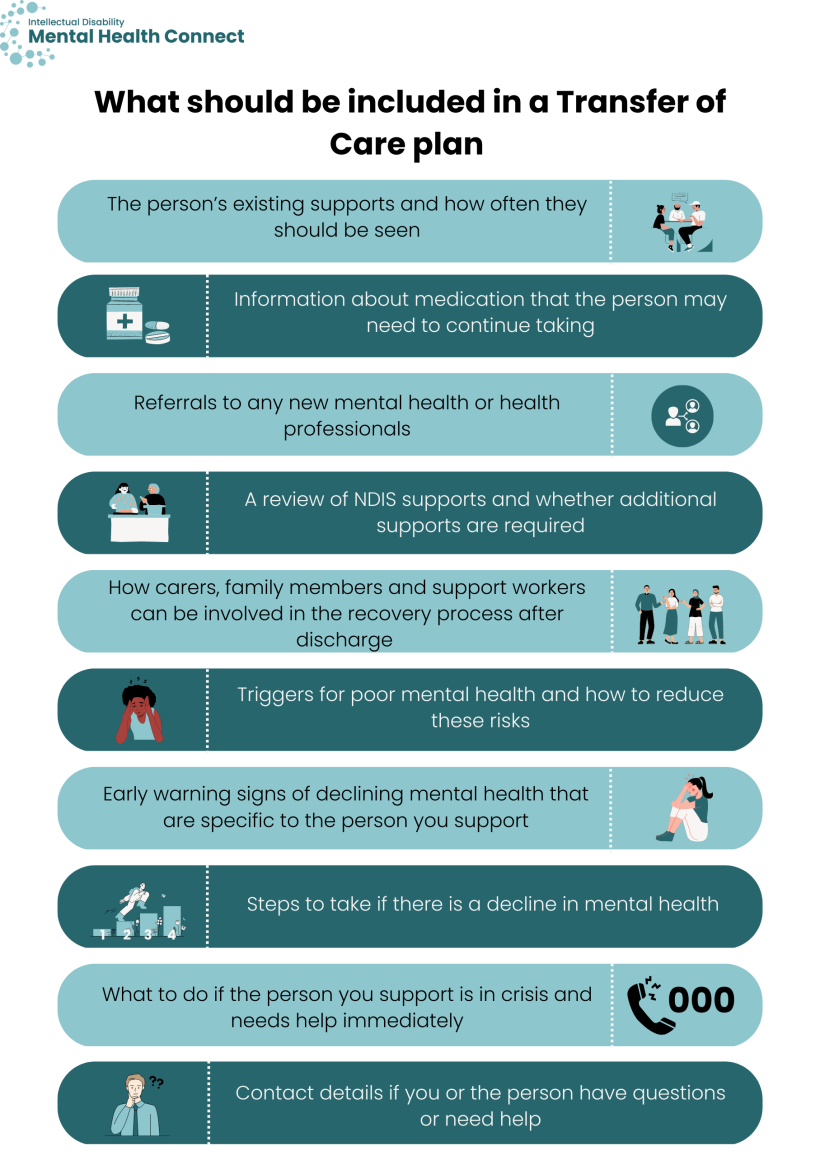
The Transfer of Care plan should include:
- the person’s existing supports and how often they should be seen
- information about medication that the person may need to continue taking. Their psychiatrist should discuss why they need to keep taking it and how to take it
- referrals to any new mental health or health professionals the person will see after they leave hospital. This could include a psychologist, community mental health nurse or psychiatrist
- a review of NDIS supports and whether additional supports are required
- how carers, family members and support workers can be involved in the recovery process after discharge (e.g. supporting coping techniques, and monitoring)
- triggers for poor mental health and how to reduce these risks
- early warning signs of declining mental health that are specific to the person you support
- steps to take if there is a decline in mental health
- what to do if the person you support is in crisis and needs help immediately
- contact details if you or the person have questions or need help.
You may find 3DN's My Easy Read discharge plan template and checklist useful.
How you can help
Consider what supports the person may need and ensure they are included in the plan
For example, if the person will need support getting to any appointments, discuss this with their mental health team. Home visits may be able to be arranged or other transport options considered.
If the person may need extra support when they leave hospital, or could benefit from care coordination, discuss whether a support worker, case manager or care co-ordinator might be helpful.
Ask questions
Ask any questions you may have and ask for written information that is accessible to the person and yourself and other members of their support networks. Make sure that the person is involved in the creation of the plan as much as possible.
Prepare for helping to monitor the person’s treatment and recovery
It is important that the person’s support networks are involved in monitoring the person’s recovery. Carers, family members and support workers can help with monitoring by recording information and asking for an unscheduled follow-up when necessary, for example if the person is experiencing ongoing medication side effects. You can discuss with the mental health professional what information to record, but important things to record may include:
- medication use and response
- side effects
- mood and behaviours
- how the person is going with using coping strategies.
It is also important to know about specific early warning signs and possible ways to respond. These should be in the person’s Transfer of Care plan, but you can ask the mental health team for more information if needed.
How you can support the person to stay well

- Support the person to attend follow-up appointments and be available for any calls or home visits from mental health professionals.
- Support the person to keep taking their medication and monitor for side effects and effectiveness. If you have questions or feel a medication review is needed, speak to the person’s GP or psychiatrist.
- Support and reinforce any tools and techniques the person has learnt during psychological therapy.
- Help the person to connect with family and friends, if that will help them.
- Support the person to take part in activities they enjoy. You can also suggest community or sports groups they may be interested in joining.
- Remember to take care of yourself. Supporting someone who has come home from hospital can be stressful. Take time for yourself when you can and seek additional support if needed (e.g. assistance from support workers). There are people you can talk to if you need help yourself. See the Looking after myself section for more information.
Professionals and services who can help after discharge
There are many professionals and services who can help after the person you support has been discharged, including community mental health centres, private psychiatrists and psychologists, rehabilitation services, and community mental health organisations. For more information, see the Services for mental health section. There are also:
What happens when the person you support feels well again?
If a person has been unwell for some time, it can be an adjustment when they start to feel well and return to work and hobbies. When the person you support returns home, they may choose to go back to the same activities they used to do. However, some people may choose to make changes in their life. For example, they may:
- find and start a new job
- decide to study
- start new hobbies.
They may need support to make these changes in their life. More information about support services that people may require when they return home can be found in the Services for mental health section.
If the person is in crisis and needs immediate help, they can:
- call 000 for an ambulance
- go to an emergency department at a hospital
- call Lifeline on 13 11 14
- ring the NSW Mental Health Line on 1800 011 511 any time, on any day, if you need to speak with a mental health professional. The mental health professional will ask you questions about the person you support’s mental health and what sort of help they need. They may refer them to the local mental health team or they may give you information and contact details about other services that can help them.
If the person is not in crisis, you can:
- follow the steps outlined in their Transfer of Care plan
- encourage the person to talk to you or another person who they trust
- encourage the person to make an appointment with their GP or another appropriate member of their mental health team
- encourage or support the person to make an emergency card.
To learn more about how to support a person in a mental health crisis, 3DN’s Intellectual Disability Health Education has an e-learning course for disability support workers. The course is available to access for a small fee.
Transitions
There are times in life when the person you support may transition between services or need different types of support. These include when they become an adult and when they become an older adult.
Disability support workers can find more information about providing mental health support to people with intellectual disability through transitions and life events in a course by 3DN’s ID Health Education. The course is available to access for a small fee.
If the person you support attends a child and adolescent mental health service, they will need to move to adult services around the time they turn 18 years old.
- Child and adolescent services are often well co-ordinated and have a multidisciplinary team. Adult services and professionals are often less co-ordinated and more likely to work independently.
- Planning for moving to adult services should start early.
- The young person’s mental health professionals should discuss the most appropriate adult services. If it is OK with the young person and their parent or guardian, they could also help with finding a service, getting an appointment and talking with the person’s new mental health professional.
- With consent, the current mental health service should transfer any health records to the new service.
- It can be helpful to arrange a meeting with both the young person’s current and new mental health professionals.
- It can be helpful if the person you support attends one or more appointments at the adult service while they are still seeing their child and adolescent mental health professional. By doing this, the young person can discuss how it went, if they are happy with the new service and talk about any issues that need to be resolved.
How you can help
Be involved in planning
Family members and support networks should all be involved in planning. It is also important for the young person to be involved in the planning. You can ask if there is a key coordinator who will help with the transition.
Promote independence
To help the person you support prepare for moving to an adult service, you could encourage them to start writing down their appointments or making their own appointments. If you or another supporter usually attends sessions with the young person, you could encourage them to try talking to the mental health professional alone for part of the session if they are comfortable with this.
Planning for getting older is important. People often wonder where they will live when they get older and who will care for them if their parents or other supporters are unable to care for them anymore. It is helpful to speak to the person you support about any questions they may have and make a plan.
For more information about transitioning to services for older people, see the Moving to new services in the section for People with intellectual disability. These resources may also help:
If the person you support uses mental health services, there are some services that provide specialised care for older persons. There is more information at NSW Health.
Resources
- 3DN's My Easy Read discharge plan template and checklist
- 3DN’s Intellectual Disability Health Education course on how to support a person in a mental health crisis.
- Disability support workers can find more information about providing mental health support to people with intellectual disability through transitions and life events.
- NSW Mental Health programs
- NSW Health Information on NSW Health mental health services and programs for older people.