Working together with the person and their team
Jump to a section below
Key points
- People with intellectual disability have the right to person-centred care and independence which means they should be included in discussions about their mental health and supported to make decisions where possible.
- Carers, family, guardians, and support workers (sometimes known as a person’s support network) also have a key role in supporting the person on their mental health journey.
- People with intellectual disability speak of the importance of professionals actively working with them and their support networks to support their mental health. [1] All can work together as a team.
- You can discuss with the person how their team can work together to best support them, including why working together is beneficial, what this may involve, and how they can communicate their preferences to their professionals.
Why is working together important to support mental health?
People with intellectual disability often have multiple people in their team who support their mental and physical health. Their team includes people such as:
- carers
- family members
- their guardian
- friends
- support workers
- mental health professionals
- other disability professionals
- advocates. An advocate is someone who speaks up to assist someone get the support they need.
As people with intellectual disability can have complex health needs, they may have multiple care plans and treatment approaches, which can lead to confusion if not well co-ordinated. When the person, their support networks and professionals work together, it helps to ensure that:
- everyone is working towards similar goals within their different roles
- each person can share their unique knowledge, skills, and ideas
- the same information does not need to be repeated to multiple professionals
- there are opportunities to share relevant health and personal history to help inform the person’s care
- care plans are clear and do not contain conflicting advice from different professionals
- each person knows who is providing what type of care so there is no overlap.
Working together can help a person with intellectual disability to recover and have good mental health.
Supporting a person with intellectual disability to be included in their mental health care
People with intellectual disability should be seen as an expert in their own life. [2] Their support networks have a key role in contributing valuable knowledge about the individual and their perspective, while professionals share their knowledge around managing mental health conditions.
There is also additional information on supporting a person across a care pathway in the Professionals’ sections Overview of care pathways for people with intellectual disability and Role of disability services.
Concerns about including people with intellectual disability in discussions about their mental health
Some carers, family members and support workers tell us that they do not include the person they support in discussions or decisions about their mental health care as they are concerned that they:
- will not understand the information
- will not be able to make a decision
- will experience anxiety.
These are all valid concerns, and all people will differ in their ability and desire to be included in discussions and decisions about their mental health. However, as people with intellectual disability have a right to be included in their mental health care, it is important to consider ways the person can be supported to make decisions in a way that is right for them. See the next section for some ideas.
How you can support a person to be included in their mental health care
You can support a person with intellectual disability by:
- providing information in an accessible format that is right for them, for example:
- Easy Read information (and supporting them to understand it)
- using pictures or symbols
- verbally
- writing notes that they can refer to later.
3DN have a Making mental health information accessible for people with intellectual disability Toolkit. While primarily aimed at health professionals, it contains practical tips for providing accessible information and supporting people to use Easy Read that you may find useful.
- providing information about tests or treatment they will have in a way that prepares them, even if it includes limited details to prevent anxiety or confusion.
- using supported decision-making to assist the person to make their own choices as much as possible. For example, discussing choices at a time of day they are most relaxed, or discussing a topic more than once before a decision is made. ADACAS Advocacy has information about supported decision-making. Even if the person has a substitute decision-maker (or is an involuntary patient or on a Community Treatment Order), their preferences should still be factored into decisions.
You can encourage the person you support to be actively involved in their mental health care planning and decisions. For example, supporting them to:
- share their communication preferences with professionals so they can participate in discussions and convey their choices
- develop and express their goals for getting well and what they want to be able to do
- prepare for appointments with their GP and mental health professionals
- monitor their treatment progress e.g. keeping a diary of any medication side effects that they can take to their GP or psychiatrist appointment.
How support networks can be included in the person they support’s mental health care
Support networks have a valuable role in working with the person with intellectual disability and their team through all stages of a mental health pathway. It is important for support networks to work with the person with intellectual disability and their team considering:
- the preferences of the person with intellectual disability
- their level of intellectual disability and communication needs
- the impact of the mental illness on the person’s functioning (and how this may differ day to day)
- legal requirements e.g. where they are the person’s guardian.
Discuss with the person you support how you could be involved and what their preferences are. This may differ for mental health compared to physical health care. For example, they may want to speak to a mental health professional alone for part of their session. It is good to plan ahead and have this conversation when the person is experiencing good mental health so that a plan is in place in the event that they become unwell.
There are many ways support networks can be involved throughout a mental health pathway. Below is a summary, with more information available in Supporting someone along a mental health pathway.
As an advocate for the person to help them to have their voice heard and needs met. This may include supporting them to seek assistance for their mental health, finding a service that has experience in intellectual disability mental health, and seeking an alternative referral if they are unable to access a particular service.
When a person is first referred to a service (this is sometimes called the intake stage) and during their assessment, support networks can:
- create a folder of the person’s referral letters, reports, medical history, and results of tests and assessments to take to appointments, or use resources such as 3DN’s My Mental Health Passport, the Council for Intellectual Disability’s My Health Matters folder, the A2D Together Folder, or Queensland Health’s Julian’s Key
- share the person’s communication preferences with professionals and other supports (e.g. using the My Health Matters folder)
- provide information on the person’s medical history, such as what is normal for them with regard to their behaviour and mood and what has changed
- share coping strategies that have worked in the past and their strengths.
During a person’s treatment, as a supporter you can:
- let mental health professionals know your experience supporting the person’s (or others’) mental health and treatment in the past. People’s familiarity with mental health varies widely. Professionals can then tailor the information they provide so it is right for you.
- take part in discussions about the person’s care plan and be provided with a copy of the plan which includes e.g. a summary of agreed upon steps, your role, and when and how to seek help if required
- assist the person to practise and use coping mechanisms at home (e.g. encouraging relaxation techniques)
- help to monitor their progress e.g.
- keep a diary of how they are finding coping strategies – see 3DN’S Coping strategy diary that can be used by supporters
- support the person to keep a diary of medication side effects – see 3DN’s Easy Read Medication side effects diary. There is also a side effects tracker and other medication templates on this page.
Supporters have a particularly important role at times when a person with intellectual disability moves between services.
- If the person you support is in hospital, you can take part in discussions around how they will be supported when they leave hospital at discharge.
- Carers and family also have an important role at times of transition, for example when a person with intellectual disability moves from child and adolescent to adult mental health services.
- More information can be found in the Supporting someone along a mental health pathway – Moving on from services section.
The role of support workers for people who live in supported accommodation
Support workers have an important role to play in supporting the mental health of people they work with, especially those living in group homes or Supported Independent Living accommodation. They may have multiple roles including:
- accompanying the person to mental health appointments
- supporting them to take and monitor medication
- supporting coping techniques.
It is important that support workers take a proactive role when asked to support a person to attend an appointment with their GP or mental health professional. This may include:
- becoming familiar with the person’s mental health history and their current concerns or treatment
- collating any information that would be beneficial to take to the appointment e.g. their behaviour support plan, monitoring sheets
- speaking to the person’s other support workers who may have witnessed different e.g. behaviours or moods that should be discussed at the appointment.
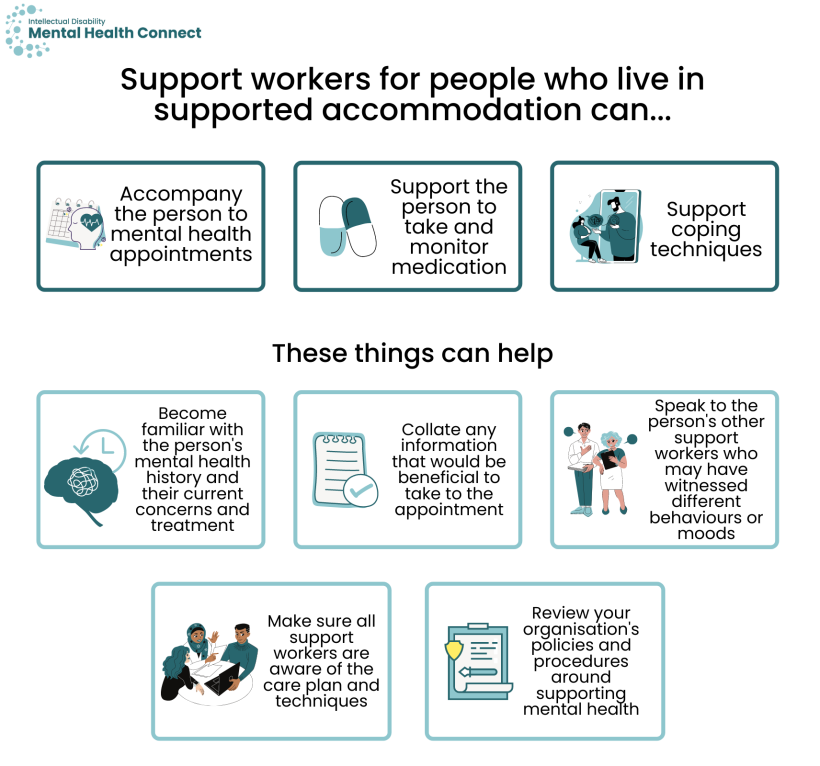
As a person with intellectual disability may have multiple support workers, it is important that they communicate and work together so all are aware of the person’s recent mental health, their care plan, and use consistent support techniques and language to describe coping skills.
Support workers should review their organisation’s relevant policies and procedures around supporting the person’s mental health.
Working together with the person you support and their professional team
The responsibility often falls to carers and family members to co-ordinate complex care for the person they support. Support networks speak of the time and considerable stress of co-ordinating care across services. This includes:
- finding suitable professionals
- providing information multiple times to multiple services
- relaying information, reports, and care plans between multidisciplinary team members.
Support networks tell us the importance of professionals working collaboratively to care for people with intellectual disability who often have complex health needs requiring multiple providers. [3] However, people with intellectual disability and their supporters tell us that their health, allied health, and disability professionals often do not work together. Many wish that their team would work more closely together.
Sometimes professionals can disagree on what treatments are best for a person with intellectual disability. Working together can help to resolve these issues.
How health and disability services can work together more collaboratively
There are multiple ways a person’s health and disability support services can work together with you and the person you support to ensure that everyone has the information that they need to support the person’s mental health.
Some ideas are provided below as to how you can encourage the person’s team to work together more collaboratively including:
- sharing information between professionals
- conducting joint assessments
- communicating more regularly
- having one care plan.

Sometimes people feel they need to repeat the same information to multiple professionals.
You could ask the health and disability professionals involved to:
- share information about the person’s health such as test results so you do not have to continually provide this information to new professionals (with the person’s or their guardian’s consent)
- use sharing software such as Google Drive or Microsoft Teams to create a virtual space for sharing information between supporting professionals (with the person’s or their guardian’s consent).
When providing information to professionals via email, it can be helpful to copy in other members of the person’s mental health care team.
Joint assessments occur when two or more members of a person’s mental health care team conduct an assessment together. For example, a psychologist and occupational therapist may co-ordinate their assessments. They may see the person at the same time or may conduct their parts of a co-ordinated assessment separately then share information afterwards (still ensuring questions are only asked once).
While joint assessments are not always possible, in certain circumstances they can help to prevent a person needing to undergo multiple assessments with different professionals. You can ask the person’s team whether this may be possible.
Many supporters say that they spend time relaying information between professionals who do not communicate with each other.
To reduce time burden, you can ask professionals to communicate more regularly and circulate information within the person’s team (with consent). This could include the following.

- Emailing updates, reports, or care plans to the person’s GP and between other team members (they can also, with consent, copy in support network members).
- Organising regular meetings or case conferences to discuss care plans, review progress, and discuss any challenges. This could occur, for example, every three months and be:
- in person or
- via teleconferencing such as Zoom or
- via phone calls.
The person you support, you, and other support network members can be involved if you wish, and the person agrees.
- Asking professionals, e.g. their psychologist, to write a short summary of the person’s sessions and emailing it to yourself and other members of the person’s team, with consent.
- The team can also use online tools or an app to keep in contact.
It is acknowledged that some of these strategies may not be practical as additional meetings may come from the person’s NDIS budget, reducing the number of treatment sessions they can access. However, even one to two additional co-ordination meetings per year could provide considerable benefits for some people.
Many people have multiple care plans, e.g. with their psychologist, occupational therapist, and behaviour support practitioner. This can be confusing and sometimes they may contain conflicting advice.
- Ask if it would be possible for professionals involved in the person’s care to discuss and make a care plan together so all the information is in one place and clear.
- While multiple plans are sometimes unavoidable, professionals can still review the person’s other care plans, discuss the plan with the relevant professional, and ensure that advice is consistent and not conflicting.
How working together can also help in other areas
Working together can also help to address other common concerns, such as supporters feeling they need more information from professionals to support a person, that a person may have a lack of support when they leave hospital or move to a new mental health service, or that professionals require more knowledge around working with people with intellectual disability who have mental health concerns.
Some supporters report wanting more information to help the person they support or more regular feedback. With the consent of the person you support, you can:
- attend appointments to learn e.g. more about their care plan and how to support their treatment
- ask professionals for regular written feedback on their progress or to arrange ‘check-in’ meetings e.g. via Zoom or in person.
This is a common concern. You can:
- ask hospital mental health staff to speak to professionals that the person has been referred to in the community to hand over information, and to keep in contact after discharge to monitor progress
- be involved in discussing the person’s discharge plan, including NDIS supports, and your role after they leave hospital (if the person/their guardian consents).
The following advice could help health professionals learn more about intellectual disability, or disability professionals about mental health.
- If professionals are not familiar with services for people with intellectual disability, encourage them to research and connect with services in the community to develop referral lists.
- Some registered health professionals can seek advice from specialist intellectual disability mental health services. You can encourage them to find out more in the Mental health services section. Please note, specialist intellectual disability mental health services are not for the general public to contact.
Resources
- For information about supported decision-making and capacity to consent in NSW, see the NSW Trustee & Guardian website which includes a Capacity Toolkit.
- ADACAS Advocacy also has information about supported decision-making.
- Supported Decision Making, a website by WAiS has information, Easy Read resources and templates about supported decision-making.
- Monitoring diaries
- Coping strategy diary
- Easy Read Medication side effects diary
- this page has a side effects tracker and other medication templates
- Resources for summarising a person’s health information include:
- 3DN’s My Mental Health Passport
- The Council for Intellectual Disability’s My Health Matters folder
- The A2D Together Folder
- Queensland Health’s Julian’s Key
References
- Weise J, Fisher KR, Whittle E, and Trollor JN. What Can the Experiences of People With an Intellectual Disability Tell Us About the Desirable Attributes of a Mental Health Professional? Journal of Mental Health Research in Intellectual Disabilities. 2018;11(3): 183-202.
- Australian Health Ministers' Advisory Council, A National Framework for Recovery-oriented Mental Health Services: Policy and Theory. 2013, Department of Health and Ageing: Canberra.
- Weise J, Fisher KR, and Trollor JN. What makes generalist mental health professionals effective when working with people with an intellectual disability? A family member and support person perspective. Journal of Applied Research in Intellectual Disabilities. 2018;31(3): 413-22.